Table of Contents
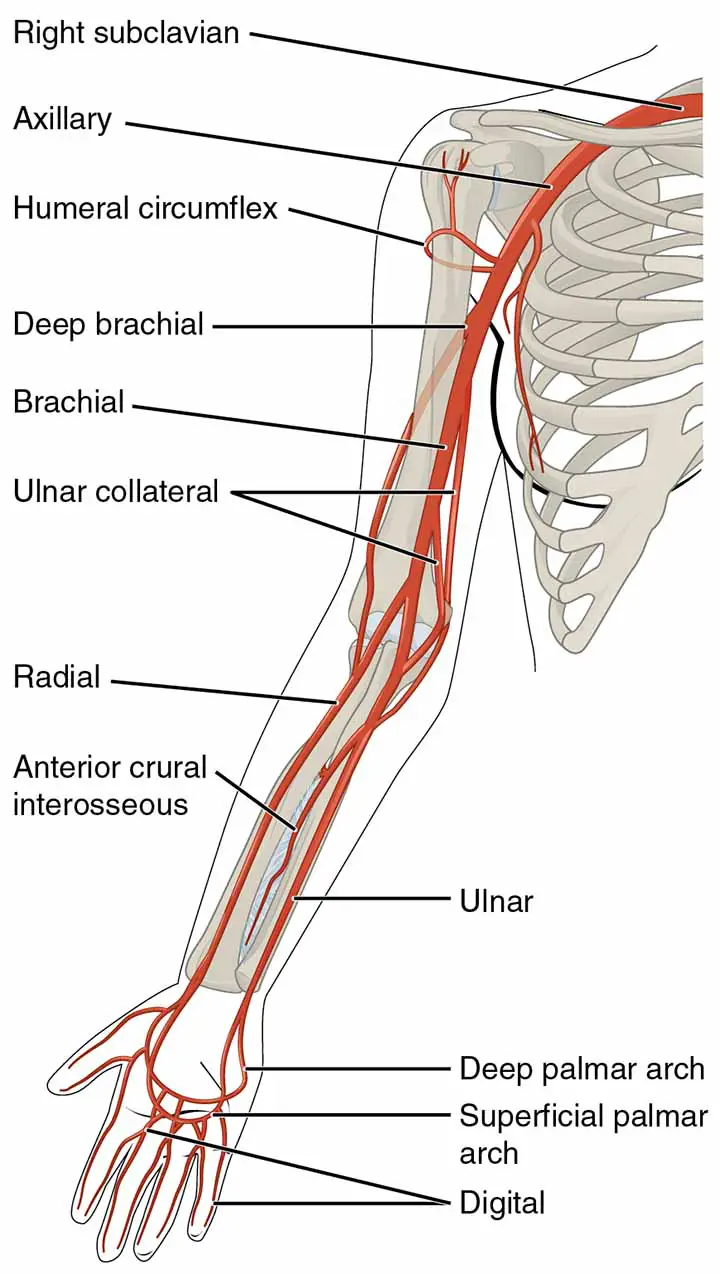
Beginning, Course, and Termination of the Ulnar Artery
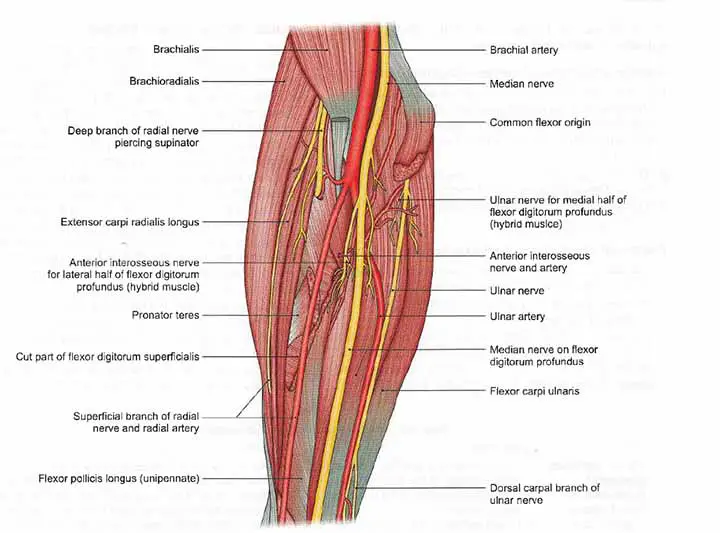
The ulnar artery, which starts in the cubital fossa, is the larger terminal branch of the brachial artery.
The artery runs obliquely downward and medially in the upper one-third of the forearm, but vertically in the lower two-thirds. It reaches the palm through the flexor retinaculum(superficially passes through it)
Relation
Anteriorly
The artery is deep in its upper half and is protected by muscles originating from the common flexor origin and the median nerve. The lower half of the artery is superficial, with only skin and fascia covering it.
Posteriorly
It is located on the brachialis and the flexor digitorum profundus.
Medially
It is related to the ulnar nerve as well as the flexor carpi ulnaris.
Laterally
It is related to the flexor digitorum superficialis
The artery is accompanied by
venae comitantes.
Read Cephalic Vein | Hand Specialist | Hand Surgeon
Branches
- Around the elbow, the anterior and posterior ulnar recurrent arteries The inferior ulnar collateral artery anastomoses with the anterior ulnar recurrent artery in front of the medial epicondyle to form the anterior ulnar recurrent artery. The larger posterior ulnar recurrent artery arises lower than the anterior and joins the superior ulnar collateral artery behind the medial epicondyle.
- The common interosseous artery (approximately 1 cm long) appears just below the radial tuberosity. It travels to the upper boundary of the interosseous membrane before splitting into the anterior and posterior interosseous arteries.
- The deepest artery on the front of the forearm is the anterior interosseous artery. It travels with the anterior interosseous nerve.
- It drops on the interosseous membrane between the flexor digitorum profundus and the flexor pollicis longus.
- It enters the extensor compartment by piercing the interosseous membrane at the upper border of the pronator quadratus.
- The artery provides muscular branches to the deep muscles of the forearm’s front, nutrient branches to the radius and ulna, and a median artery that runs alongside the median nerve.
- The posterior interosseous artery gives off the interosseous recurrent artery near its base, which runs upwards and anastomoses with the middle collateral artery (posterior branch of profunda brachii artery) behind the lateral epicondyle.
- Muscular branches supply the forearm’s medial muscles.
- The anastomoses around the wrist joint are formed by the palmar and dorsal carpal branches. The palmar carpal branch contributes to the formation of the palmar carpal arch.
The dorsal carpal branch begins just above the pisiform bone and winds backward to the tendons before terminating in the dorsal carpal arch.
This arch is developed medially by the ulnar artery’s dorsal carpal branch and laterally by the radial artery’s dorsal carpal branch.
Read The Allen’s Test
Read The Brachial Pulse
Mnemonics for remembering the branches;
Anatomical Pictures Can Definitely Deeply Please
A – Anterior ulnar recurrent
P – Posterior ulnar recurrent
C – Common interosseous artery
D – Dorsal carpal branch
D – Deep palmar branch
P – Palmar carpal branch
Surface Marking
The ulnar artery is marked by joining the following points;
- A point in front of the elbow at the level of the radius neck medial to the biceps brachii tendon.
- A second point is located at the intersection of the upper one-third and lower two-thirds of the forearm’s medial border (lateral to the ulnar nerve).
- The third lateral point to the pisiform bone. As a result, the ulnar artery’s direction is oblique in the upper one-third and vertical in the lower two-thirds.
In the lower two-thirds of its path, the ulnar nerve runs just medial to the ulnar artery.
The ulnar artery continues in
the palm(hand)
as the superficial palmar arch.
Read The Styloid Process of Ulna
Ulnar Artery On Hand
This artery’s route in the forearm has already been represented. It enters the palm(hand) superficially to the flexor retinaculum but deep to the volar carpal ligament. It then divides into the superficial palmar branch, which is the artery’s central continuation, and the deep palmar branch. These branches help to develop the superficial and deep palmar arches, respectively.
Superficial Palmar Arch
The arch is a vital anastomosis between the ulnar and radial arteries.
The arch’s convexity is oriented toward the fingers, with its most distal point at the level of the distal border of the completely extended thumb.
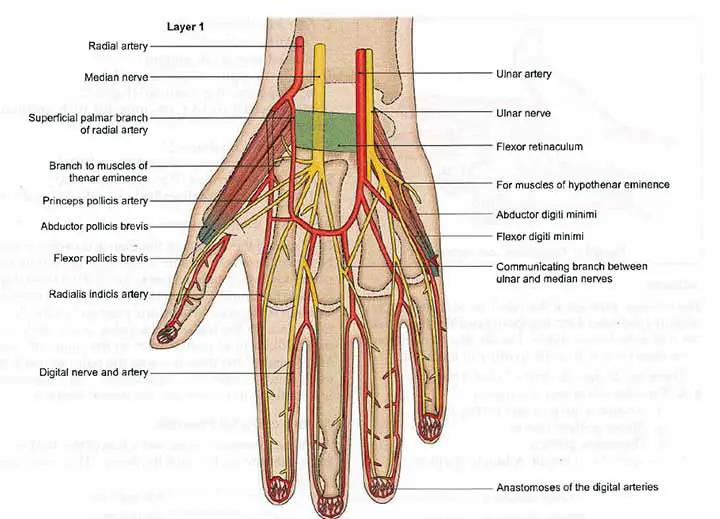
Formation
The superficial palmar arch is created by the superficial palmar branch, which is a direct continuation of the ulnar artery beyond the flexor retinaculum. The arch is completed on the lateral side by the superficial palmar branch of the radial artery.
Relations
Deep to the palmaris brevis and the palmar aponeurosis is the superficial palmar arch. It runs over the palm, passing over the flexor digiti minimi, flexor tendons of the fingers, lumbricals, and digital branches of the median nerve.
Branches
The medial 3.5 fingers are supplied by 3(three) common digital and one proper digital branch from the superficial palmar arch. The corresponding palmar metacarpal arteries from the deep palmar arch connect the lateral 3(three) common digital branches.
The deep branch of the ulnar artery emerges directly in front of the flexor retinaculum, just above the pisiform bone. It soon joins and completes the deep palmar arch by passing between the flexor and abductor digiti minimi.
Read The Axillary Artery
Clinical Anatomy
Operation in hand
Adrenaline is not recommended for use in hand procedures since the proper digital arteries are small end arteries that are vulnerable to vascular spasm and necrosis if left constricted for too long. Since the arteries that supply the fingers and toes are small and vulnerable, frostbite affects them first.
Hypothener Hammer Syndrome
Hypothenar hammer syndrome is a hand disorder in which blood flow to the fingers is limited. The group of muscles that control the movement of the little finger is referred to as the hypothenar. Any of these muscles are responsible for the fleshy edge of the hand (hypothenar eminence). It occurs when workers repeatedly use their palms (particularly the hypothenar eminence) as hammers to grind, push and twist hard objects. These activities have the potential to harm certain blood vessels in the hand, especially the ulnar artery. This artery runs through the palm’s hypothenar region and delivers blood to the fingers. Blood flow to the fingers is reduced when the ulnar artery is damaged. Hypothenar hammer syndrome may be caused by a single significant episode.
Hypothenar hammer syndrome is most common in men over the age of 40. Auto mechanics, metal workers, lathe operators, miners, machinists, butchers, bakers, carpenters, and bricklayers are among those at risk. Vibrating tool operators are also at risk. Sports such as karate, baseball, mountain biking, golf, tennis, hockey, handball, volleyball, badminton, break-dancing, and weight lifting have also been linked to hypothenar hammer syndrome.
Symptoms
Pain over the hypothenar eminence and ring finger, pins and needles (paresthesia), loss of feeling, and trouble keeping heavy objects in the affected hand are all symptoms of hypothenar hammer syndrome. The fingers become cold-sensitive and change color.
Treatment
The first step in treating hypothenar hammer syndrome is to stop the behaviors that caused the syndrome. Other measures can include quitting smoking (smoking reduces blood circulation), wearing padded protective gloves, and avoiding cold weather. Certain medications will aid in the restoration of blood flow.
Surgery may be needed
in some cases.
Arterial Blood Gas(ABG)
Blood gas analysis is a widely used diagnostic technique for determining the partial pressures of gases in the blood as well as the acid-base material. The understanding and application of blood gas analysis allow providers to interpret pulmonary, circulatory, and metabolic disorders.
A “blood gas analysis” can be performed on blood drawn from any location in the circulatory system (artery, vein, or capillary). An arterial blood gas (ABG) test specifically measures blood drawn from an artery. ABG testing determines a patient’s partial pressure of oxygen (PaO2) and carbon dioxide (PaCO2) (PaCO2). PaO2 indicates the status of oxygenation, while PaCO2 indicates the status of ventilation (chronic or acute respiratory failure). Hyperventilation (rapid or deep breathing), hypoventilation (slow or shallow breathing), and acid-base status all have an effect on PaCO2. While pulse oximetry and end-tidal carbon dioxide monitoring can be used to evaluate oxygenation and ventilation non-invasively, ABG analysis is the gold standard.
Most ABG analyzers specifically calculate pH and PaCO2 when determining acid-base balance. The serum bicarbonate (HCO3) and base deficit or surplus was calculated using a derivative of the Hasselbach equation. This formula always yields a difference from the calculated value due to the equation’s failure to account for blood CO2. A solid alkali is used to test HCO3, which liberates all CO2 in serum, including dissolved CO2, carbamino compounds, and carbonic acid. The estimate only takes into account dissolved CO2; this measurement using normal chemistry analysis would most likely be referred to as “absolute CO2.” As a result, the difference would be about 1.2 mmol/L. However, a greater difference between the ABG and the measured value can be seen, particularly in critically ill patients.
Based on the sample, unit, or calibration used, the measurement has been contested as both correct and inaccurate and must be interpreted correctly based on the institutional standards.
Arterial blood gases are often ordered by emergency medicine, intensive care medicine, anesthesiology, and pulmonology physicians, but they may also be required in other clinical settings. An ABG is used to diagnose a variety of diseases, like acute respiratory distress syndrome (ARDS), extreme sepsis, septic shock, hypovolemic shock, diabetic ketoacidosis, renal tubular acidosis, acute respiratory failure, heart failure, cardiac arrest, asthma, and inborn metabolic errors.
Read The Radial Artery
Ulnar Artery Thrombosis
Ulnar artery thrombosis (UAT) is most common in athletes and manual laborers who use their palms repeatedly in high-impact activities. Anecdotal evidence suggests that orthopedic surgeons, especially joint arthroplasty surgeons, have a higher prevalence of UAT than the general population. This study aimed to find out how common UAT is among orthopedic surgeons and to identify risk factors for developing UAT. The research included 80 orthopedic surgeons and residents. A demographic questionnaire was completed by each participant, and a timed Allen test was performed on each hand with the radial artery occluded. A reperfusion time of more than 6 seconds was deemed abnormal. Participants who had a positive Allen test and UAT-related symptoms were diagnosed with UAT.
Takeaway
The ulnar artery is the largest branch of the brachial artery. It contributes to forming the superficial palmar arch. It has significant clinical importance.
Last Updated on February 23, 2022 by Learn From Doctor Team