Table of Contents
Axillary Artery Overview
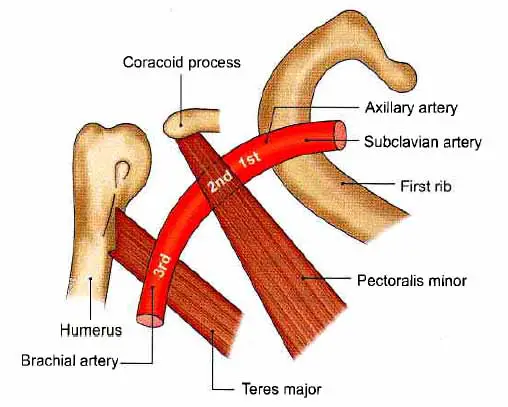
The axillary artery is a terminal branch(continuation) of the subclavian artery. It runs from the first rib’s outer border to the teres major muscle’s lower border, where it becomes the brachial artery. Its orientation changes depending on the location of the limb.
The artery is divided into three parts by the pectoralis minor muscle, which crosses it.
- 1st part, The superior (proximal) to the muscle.
- 2nd part, which is posterior (deep) to the muscle.
- 3rd part, inferior (distal) to the muscle.
Relation
1st Part Relation
Anterior
- Skin
- The superficial fascia and platysma, supraclavicular nerves
- The deep fascia
- The clavicular segment The lateral thoracic of the pectoralis major muscle
- The clavipectoral fascia and cephalic vein, lateral pectoral nerve, thoracoacromial artery.
- The communication loop between the lateral and medial pectoral nerves
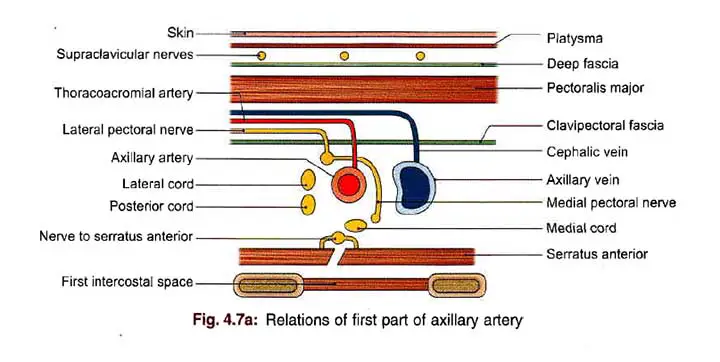
Posterior
- The first intercostal space along with the external intercostal muscle
- The nerve to the serratus anterior with the first and second digits of the serratus anterior.
- Brachial plexus medial cord and its medial pectoral branch
Lateral
The brachial plexus’s lateral and posterior cords
Medial
The medial axillary vein – The first part of the axillary artery is wrapped (along with the brachial plexus) in the axillary sheath, which is derived from the prevertebral layer of the deep cervical fascia.
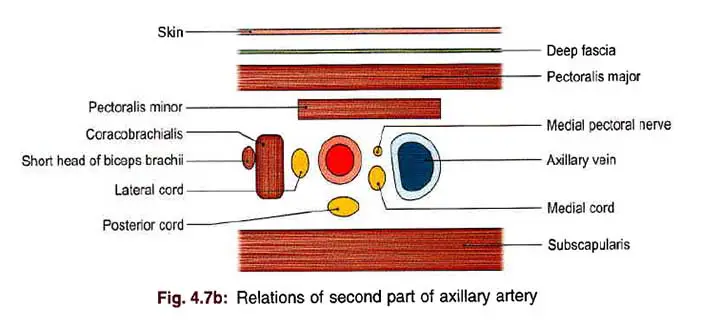
2nd Part Relation
Anterior
- Skin
- The superficial fascia
- The deep fascia
- The pectoralis major muscle
- The pectoralis minor muscle
Read The Axillary Vein
Posterior
- The brachial plexus’s posterior cords
- The subscapularis muscle
Lateral
- The brachial plexus’s lateral cord
- The coracobrachialis muscle
Medial
- The brachial plexus’s medial cord
- The medial pectoral nerve
- The axillary vein
3rd Part Relation
Anterior
- Skin
- The superficial fascia
- The deep fascia
- The pectoralis major and the medial root of the median nerve are located in the upper part.
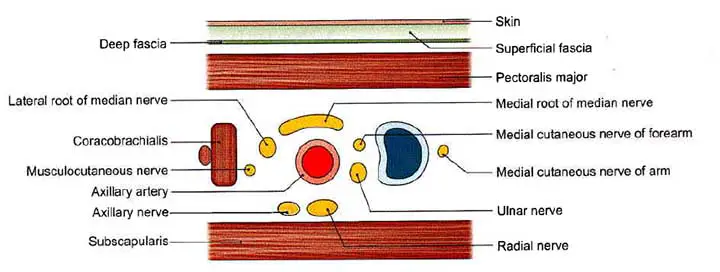
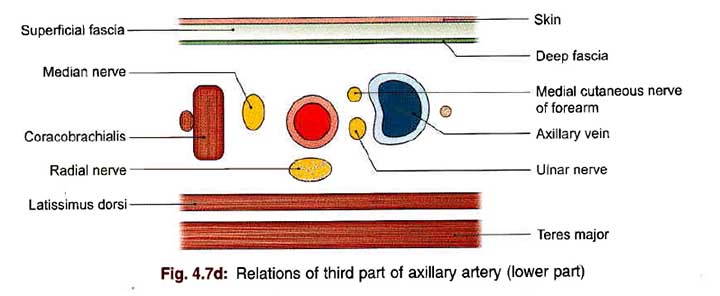
Posterior
- The radial nerve
- The axillary nerve in the upper part
- The subscapularis in the upper part
- Tendons of the latissimus dorsi along with the teres major in the lower part
Lateral
- The coracobrachialis
- The musculocutaneous nerve in the upper part.
- The lateral root of the median nerve in the upper part
- The trunk of the median nerve in the lower part.
Medial
- Axillary vein
- The medial cutaneous nerve of the forearm and ulnar nerve, between the axillary artery the axillary vein
- The medial cutaneous nerve of arm, medial to the axillary vein
Read The Radial Artery
Branch
Six branches arise from the axillary artery. One branch develops from the first part, two branches develop from the second part, and three branches develop from the third part.
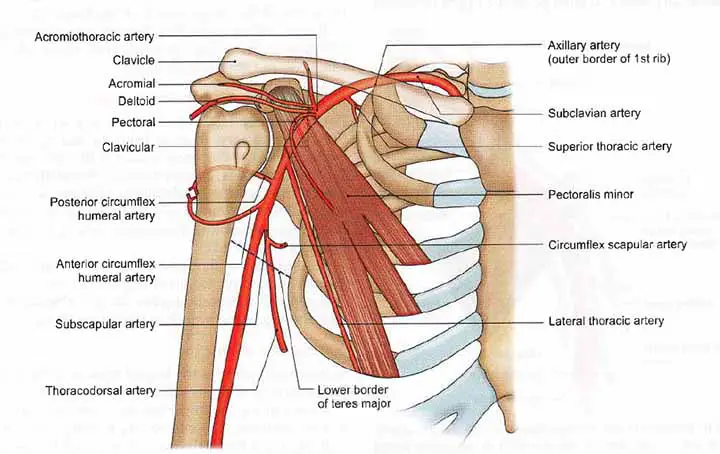
The branches are;
The Superior Thoracic Artery
The superior thoracic artery is a very small branch that develops from the axillary artery’s first part (near the subclavius). It runs downward, forward, and medially, passing between the two pectoral muscles until terminating by supplying these muscles and the thoracic wall.
Acromiothoracic (Thoracoacromial) Artery
The thoracoacromial artery is a branch of the axillary artery’s second part. It develops at the upper border of the pectoralis minor, pierces the clavipectoral fascia, and quickly divides into the four terminal branches mentioned below.
- The pectoral branch goes between the pectoral muscles and supplies these muscles along with the breast.
- The deltoid branch runs in the deltopectoral groove, together with the cephalic vein.
- The acromial branch connects the anastomoses over the acromion after crossing the coracoid process.
- The clavicular branch supplies the sternoclavicular joint and subclavius and extends superomedially deep to the pectoralis major.
Lateral Thoracic Artery
This artery is a branch of the axillary artery. It arises at the lower boundary of the pectoralis minor and passes along it, near to the anterior group of axillary lymph nodes.
The artery is wide in females and gives off lateral mammary branches to the breast.
Anterior Circumflex Humeral Artery
The anterior circumflex humeral artery is a small branch that arises from the third part of the axillary artery along the lower border of the subscapularis.
It runs laterally in front of the humerus’s intertubercular sulcus and connects with the posterior circumflex humeral artery to form an arterial loop around the surgical neck of the humerus.
It provides an ascending branch into the intertubercular sulcus, supplying the humeral head and shoulder joint.
Posterior Circumflex Humeral Artery
The anterior circumflex humeral artery is much smaller than the posterior circumflex humeral artery. It originates at the lower border of the subscapularis from the third segment of the axillary artery. It travels backward with the axillary nerve, through the quadrangular intermuscular space, and ends by anastomosing with the anterior circumflex humeral artery around the surgical neck of the humerus.
It supplies blood to the shoulder joint, the deltoid, and the muscles that surround the quadrangular space.
It provides a descending branch that connects to the ascending branch of the profunda brachii artery.
The Subscapular Artery
The axillary artery’s largest branch, the subscapular artery, arises from its third segment.
It extends along the lower border of the subscapularis to the inferior angle of the scapula.
It supplies to the latissimus dorsi and serratus anterior muscles.
It gives rise to a broad branch, the circumflex scapular artery, which is wider than the main artery’s continuation. This branch passes through the triangular intermuscular space, winds deep to the teres minor around the lateral border of the scapula, and gives a branch to the subscapular fossa and another to the infraspinous fossa, both of which participate in the anastomoses around the scapula.
Collateral Circulation and Anastomoses
The axillary artery branches anastomose with one another and with branches originating from neighboring arteries (internal thoracic, intercostal, suprascapular, deep branch of transverse cervical, profunda brachii). When the axillary artery becomes blocked, collateral circulation is formed by anastomoses around the scapula that connect the first part of the subclavian artery to the third part of the axillary artery (apart from communications with the posterior intercostal arteries).
Read The Ulnar Artery
Mnemonic to remember Axillary Artery Branches
Save The Lions And Protect Species
- Superior thoracic artery
- Thoracoacromial artery
- Lateral thoracic artery
- Anterior circumflex humeral artery
- Posterior circumflex humeral artery
- Subscapular artery
Clinical Points
Axillary Arterial Pulsation
Axillary arterial pulsations can be felt against the lower axillary lateral wall. The artery can be effectively pressed against the humerus in the lower part of the lateral wall of the axilla to stop bleeding from the distal part of the limb (in fractures, operations, and amputations).
Axillary Artery Aneurysm
True axillary artery aneurysms in children are uncommon and are usually caused by a blunt trauma on the shoulder or axilla region. Idiopathic bilateral axillary aneurysms in children are much rarer, and there is no evidence for optimal treatment. Furthermore, the longest follow-up period for procedures recorded in pediatric axillary artery aneurysms was less than a year, and long-term results were uncertain.
Axillary Artery Occlusion(AAO)
The presence of an asymptomatic AAO may alter the treatment plan, but it may be difficult to detect before surgery. In cases where a brachial or radial artery access is planned, a contrast medium should be injected from the contralateral upper extremity during preoperative enhanced CT because the absence of halation of the ipsilateral subclavian/axillary vein allows for better visualization of the AAO, which can lead to a better preoperative strategy, including the side of upper extremity access.
Cannulation
Some studies compared the early and late results of patients who had femoral artery cannulation and axillary artery cannulation for acute type A aortic dissection repair.
Result of the study shows;
Overall, 12.6 percent of patients died during surgery (axillary 15.7 percent, femoral 10.7 percent; P = 0.564). Patients undergoing axillary artery cannulation had a statistically nonsignificantly higher surgical mortality rate in both healthy and dysfunctional patients (13 percent vs. 6.5 percent, P = 0.405 and 40 percent vs. 22.7 percent, P = 0.818, respectively). Although there was no difference in major complication rates, such as stroke, poor cardiac performance, and surgical revision for bleeding/tamponade, patients who underwent axillary cannulation had a higher incidence of renal failure that needed dialysis (12 percent vs. 1%, P = 0.022). Multivariate analysis revealed that hemodynamic instability on admission (OR 3.87; 95 percent CI, 1.23 to 12.63; P = 0.021), lower preoperative creatinine clearance (OR 0.94; 95 percent CI, 0.90 to 0.97; P = 0.001), and use of axillary artery stent were predictors for the composite endpoint of operative mortality or severe organ malperfusion, such as renal failure or cerebrovascular accident. The 3-year survival rate for those discharged from the hospital was 91 percent in the axillary group and 87 percent in the femoral group ( P = 0.772).
Injury
Traumatic axillary artery lesions are uncommon, accounting for just 15 to 20% of upper limb arterial injuries. The majority of the traumas are caused by penetrating wounds, with the remaining 6% caused by blunt traumas following shoulder fracture-dislocations. The axillary artery is often ruptured in high-energy accidents around the shoulder girdle, which are associated with multiple nerve ruptures, the frequency of which varies from 27 to 44 percent. Distal ischemia can result from the injured axillary artery. As a result, it is hypothesized that vascular repair via interposition grafting should be the preferred treatment. It is unclear if the injured axillary artery can be reconstructed in patients that have perfectly viable distal limbs due to an extensive anastomotic network of collateral arteries. Some research describes three cases of proximal humeral fractures caused by axillary artery damage that were treated with or without artery reconstruction.
Axillary Artery Summery
The axillary artery is a broad muscular artery that runs through the axilla. It is in charge of transporting oxygen-rich blood to the upper limb, as well as portions of the scapula and upper lateral thorax’s musculocutaneous system.
Last Updated on February 23, 2022 by Learn From Doctor Team