Table of Contents
Axillary Vein Overview
The axillary vein is the basilic vein’s continuation. A little above the lower border of the teres major, the axillary vein is joined by the venae comitantes of the brachial artery. It is located on the axillary artery’s medial side. It becomes the subclavian vein at the outer border of the first rib. It receives the cephalic vein in its upper part, in addition to the tributaries corresponding to the branches of the axillary artery.
There is no axillary sheath surrounding the vein, allowing it to extend during periods of increased blood flow.
Origin: The union of the paired brachial veins and the basilic vein gives rise to it.
Course: It extends medially to the axillary artery in the axillary region.
Drainage: The axilla, upper limb, and chest wall (superolateral)
Tributaries: comprise the cephalic vein and five other tributaries that correlate to axillary artery branches.
Termination: at the lateral border of the first rib, it continues with the subclavian vein.
Detailed Anatomy
The axillary vein is an upper limb deep vein developed by the union of the brachial and basilic veins. It begins at the teres major muscle’s lower border and ascends medially through the axilla to the first rib, where it is connected by the subclavian vein.
The axillary vein runs anteromedial to the axillary artery, partly overlapping it. The subscapular, circumflex humeral, lateral thoracic, thoracoacromial, and cephalic veins are tributaries of the axillary vein, and the majority of them correspond to branches of the axillary artery.
Course
The axillary vein arises from the confluence of the brachial and basilic veins at the lower border of the teres major tendon. It travels upwards and medially through the axillary area (armpit). The axillary vein then travels to the lateral border of the first rib, where it becomes the subclavian vein.
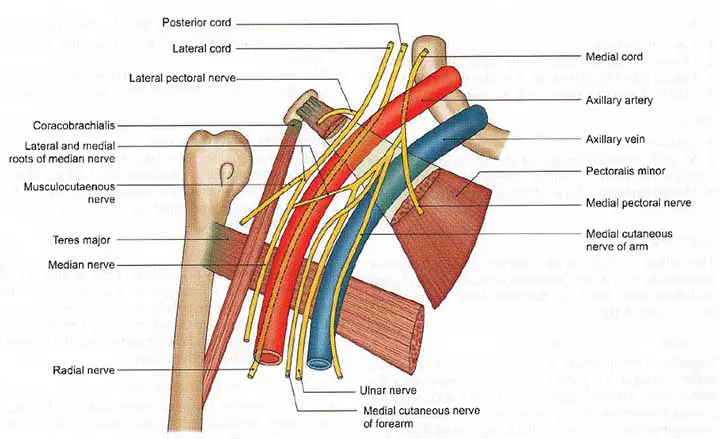
The axillary vein travels alongside the axillary artery through the armpit area. It runs on the artery’s anteromedial side, partly overlapping it. The axillary artery and vein form a bundle with many neurovascular structures of the axilla, including the lateral and medial pectoral nerves, the brachial plexus medial cord, the ulnar nerve, and the medial cutaneous nerve of the arm.
The axillary vein receives tributaries that lead to axillary artery branches. These veins are known as the subscapular, circumflex, humeral, lateral, and thoracoacromial veins. Furthermore, the axillary artery receives the cephalic vein at its terminus.
Read The Cephalic Vein
Anatomical Points
Origin
The axillary vein is created by the union of the paired brachial veins (venae comitantes of the brachial artery) and the basilic vein at the inferior border of the axilla.
Course
As mentioned in the above discussion.
Divisions
The axillary vein, like the axillary artery, can be divided into three sections based on its relation to the pectoralis minor (above, behind, or below)
Tributaries
The axillary vein’s second and third parts have tributaries that correspond to axillary artery branches. These are the thoracoacromial vein, lateral thoracic vein, subscapular vein, anterior circumflex humeral vein, and posterior circumflex humeral vein.
The cephalic vein joins the vein after piercing the clavipectoral fascia and is a tributary of the first part of the axillary vein (above the pectoralis minor muscle).
Termination
The axillary vein becomes the subclavian vein at the lateral border of the first rib and continues as the subclavian vein.
Drainage
Deoxygenated blood is drained from the arm, axilla, and superolateral chest wall through the axillary vein. It also receives contributions from the anterolateral abdominal wall’s thoracoepigastric vein.
Read The Basilic Vein
Clinical Points
Axillary Vein Cannulation
In terms of infection rate, patient comfort, and anatomical relationship with the clavicle and lungs, the axillary vein is a good site for ultrasound-guided central venous cannulation. In one research, real-time ultrasound-guided axillary vein cannulation was compared to traditional infraclavicular landmark-guided subclavian vein cannulation in infants. In one sample, 132 paediatric patients were randomly assigned to either ultrasound-guided axillary vein (axillary group) or landmark-guided subclavian vein (subclavian group) (landmark group). The outcomes calculated were the success rate after two attempts, the success rate on the first attempt, the time to cannulation, and the complication rate. The axillary group had an 83 percent success rate after two attempts, while the hallmark group had a 63 percent success rate (odds ratio 2.85, 95 percent CI 1.25-6.48, p = 0.010). The axillary group had a 46 percent first-attempt success rate and a 40 percent landmark group success rate (p = 0.274), and the median time to cannulation was 156 seconds for the axillary group and 180 seconds for the landmark group (p = 0.286). There were no variations in complication rates between the two groups, while the hallmark group had three incidents of subclavian artery puncture (p = 0.08). We conclude that in pediatric patients, axillary vein cannulation using a real-time ultrasound-guided in-plane technique is useful and efficient.
Axillary Vein Entrapment
A patient with right axillary vein obstruction due to compression of the vein caused by anomalous muscle tissue extending from the latissimus dorsi muscle through the neurovascular bundle to the pectoralis major muscle was studied. Just a few cases of this ‘axillopectoral muscle’ causing axillary vein entrapment have been identified. These previous studies are examined in detail, with a focus on the symptoms and phlebographic findings. The obstruction and the symptoms it causes are sporadic, but the phlebographic characteristics are distinctive.
Axillary Vein Thrombosis
Acute swelling and discomfort in the upper limb caused by thrombus occlusion of the axillary and/or subclavian veins. This can happen as a consequence of a primary phenomenon or as a result of secondary causes like an indwelling venous catheter, thrombophilia, or thoracic outlet syndrome.
Signs and Symptoms
- Patients usually present with hand pain and swelling, as well as discoloration.
- 3-36 percent of cases can result in pulmonary embolism, which is characterized by pleuritic chest pain, shortness of breath, and hemoptysis.
- The physical examination can reveal a low-grade fever as a result of thrombus formation. Higher fevers are seen in patients with septic thrombophlebitis or in those that have a malignancy.
- Arm and hand edema
- Cyanosis of the hand
- Dilated superficial collateral veins over the chest and upper arm can be the only sign of central venous cannulation.
- There is fullness in the supraclavicular fossa as well as a palpable cord of the thrombosed vein.
- The jugular vein may be dilated.
Treatment
Acute anticoagulation (low molecular weight heparin, fondaparinux, intravenous/subcutaneous unfractionated heparin) is advised. It is preferable to use low molecular weight heparin or fondaparinux. Rivaroxaban and apixaban are also options.
Variation of Axillary Vein and its Tributaries
The anatomy and variations of the axillary vein have major consequences in invasive procedures such as venous access, axillary block, arteriovenous fistula formation, axillary node dissection, breast augmentation, and other axillary surgical procedures. To better understand the anatomy of the axillary vein and its tributaries, 40 cadaveric upper extremities were dissected and divided into multiple groups based on the courses and terminations of brachial veins. The brachial veins either ended separately (Type A; 72.5 percent ) or joined together (Type B; 27.5 percent ) to meet the basilic vein or the axillary vein. In 5.0 percent of the cases, the basilic vein was missing. The axillary vein was found to be duplicated in 17.5 percent of the specimens, and the lateral venous channel running along the lateral wall of the axilla was found to be duplicated in 40.0 percent of the specimens. The lateral brachial vein was the most common drainage vein of the deep brachial vein (67.5 percent ). In 67.5 percent of the cases, the anterior circumflex humeral vein also empties into the lateral brachial vein. The posterior circumflex humeral vein crossed the brachial plexus and connected to either the axillary vein (45.0 percent) or the subscapular vein (42.5 percent ). In 15.0 percent of the cases, a lateral brachial vein, a normal brachial vein, or a venous channel perforated the lateral root of the median nerve.
Summery
The axillary vein is a major vein in the upper body that transports blood to the heart from the upper limb, armpit, and upper side of the chest wall. It develops on either side of the body where the basilic and brachial veins meet in the axilla, a space just below the shoulder where arteries, veins, and nerves can pass.
Last Updated on February 23, 2022 by Learn From Doctor Team