Table of Contents
Subclavian Artery Overview
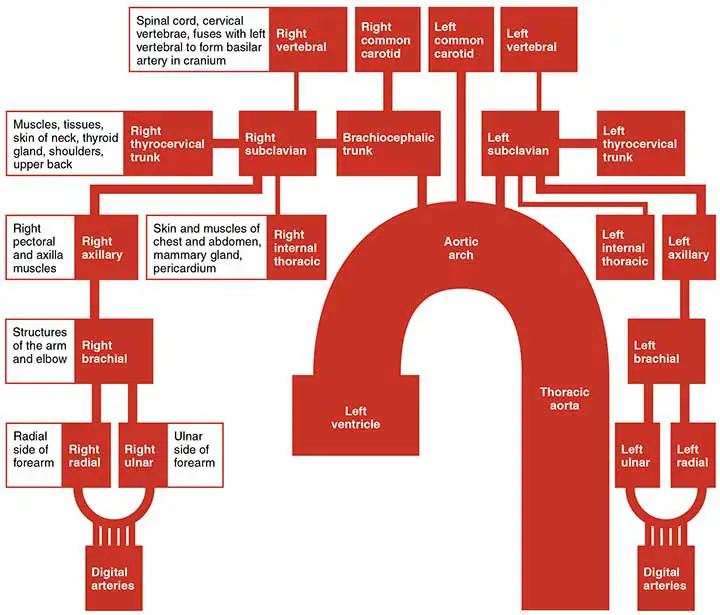
The subclavian arteries are paired asymmetric arteries and they supply blood to the posterior cerebrum, cerebellum, neck(posterior), upper limbs, and superior and anterior chest walls.
Origin
The right and left subclavian arteries are not from the same origin.
The Right Subclavian Artery: The right subclavian artery (RSA) is one of the brachiocephalic artery’s terminal branches.
The Left Subclavian Artery: After the left normal carotid artery, the left subclavian artery (LSA) develops as the third branch of the aortic arch.
Course
The subclavian artery leaves the thorax through the superior thoracic aperture between the anterior and middle scalene muscles before passing between the first and second ribs and the clavicle. It continues as the axillary artery at the lateral boundary of the first rib.
Parts of the Artery
The vessel can be divided into three sections (first, second, and third) based on its position relative to the scalenus anterior muscle.
- 1st Part: From its point of origin to the medial border of the scalenus anterior muscle.
- 2nd Part: It’s posterior to the anterior scalenus muscle.
- 3rd Part: It’s from the anterior lateral border of the scalenus to the anterior lateral border of the first rib.
Relations
Relations of 1st Part
Anterior
- The common carotid artery
- The internal jugular and vertebral vein
- The vagus and phrenic(only left side) nerve, cardiac branches of the vagus and sympathetic trunk, and the ansa cervicalis.
- Sternocleidomastoid, sternohyoid, sternothyroid muscles
- The Thoracic duct
Posterior
- The apex of the lung
- Brachial Plexus(lower trunk)
- The scalenus medius muscle
Relations of 2nd Part
Anterior
- The scalenus anterior muscle
- The phrenic nerve (only right side)
- The sternocleidomastoid muscle
Posterior
- The apex of the lung
- Brachial Plexus(lower trunk)
- The scalenus medius muscle
Relations of 3rd Part
Anterior
- The suprascapular and the transverse cervical vessels
- The subclavian and the anterior jugular vein
Posterior
- The apex of the lung
- Brachial Plexus(lower trunk)
- The scalenus medius muscle
Note: All three parts of the subclavian artery have the same posterior relations.
Branches
Three parts arise different branches.
Branches of 1st Part
- The vertebral artery runs cranially, supplying the posterior cerebral circulation.
- The Internal thoracic artery: Pathways Caudally
- The thyrocervical trunk: a very short trunk that splits quickly into four branches.
Branches of 2nd Part
- The costocervical trunk runs cranially before splitting.
Branches of 3rd Part
- The dorsal scapular artery passes posteriorly (less generally, it branches from the second part); some authors classify this branch as originating from the thyrocervical trunk.
Mnemonic of Subclavian Artery Branches
Mnemonic is the important and smartest way to remember the branches of the subclavian artery;
Very Tired Individuals Sip Strong Coffee Served Daily
- Vertebral artery
- Thyrocervical trunk
- Inferior thyroid artery
- Superior cervical artery
- Suprascapular artery
- Costocervical trunk
- Supreme intercostal artery
- Deep cervical artery
Some also try to remember with VIT C D(VITamin C D)
As we already discussed the summary of the subclavian artery for the people in a hurry, now it’s time to dive deeper into this.
Deep Anatomy of the Subclavian Artery
The subclavian arteries are two large arteries in the thorax that supply blood to the thorax, as well as the head, neck, shoulder, and arms. It may have two roots, depending on which side of the body it is on: the aortic arch on the left or the brachiocephalic trunk on the right.
The subclavian artery eventually becomes the axillary artery, the arterial supply to the upper limb regardless of which side of the body it is on. It splits into several branches along its route, one from each of its three regions: thoracic, muscular, and cervical. There are a total of eight branches.
The course of the Artery
The subclavian artery develops directly from the aortic arch on the left side of the body, while it arises from the brachiocephalic trunk on the right. Both run above the cervical pleura, across the posterior scalene gap, and through the anterior scalene muscle (between the anterior and medial scalene muscles). The axillary artery develops at the axilla between the first rib and the clavicle.
Branches of the Subclavian Artery
Thoracic Region
It originates plenty of branches along the way. The following thoracic branches develop medial to the scalenus anterior muscle.
The Vertebral Artery
The first branch is the vertebral artery, it rises until it passes the vertebral column via the transverse foramen of the sixth or seventh cervical vertebra.
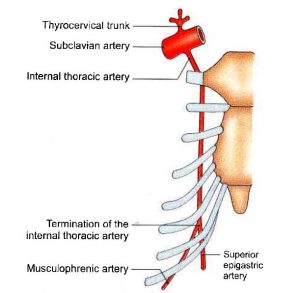
The Internal thoracic artery
The second is the internal thoracic artery, which passes behind the sternum and costal cage in the same direction as the vertebral artery. It divides into three smaller arteries;
- The superior epigastric artery appears and passes under the costal margin before accessing the rectus sheath.
- The pericardiacophrenic artery runs alongside the phrenic nerve between the pleura and the pericardium, supplying the fibrous pericardium. It joins the musculophrenic and superior phrenic arteries.
- The musculophrenic artery supplies the diaphragm’s upper muscles.
The Thyrocervical Trunk
The third artery is the thyrocervical trunk, which ascends with four branches.
- The inferior thyroid artery ascends and loops behind the normal carotid artery, and travels to the thyroid’s backside, crossing the recurrent laryngeal nerve. It sends arteries to the larynx (inferior laryngeal artery), infrahyoid muscles, and prevertebral muscles, as well as several smaller arteries to the surrounding structures.
- The ascending cervical artery continues, ascending along the phrenic nerve at the fourth cervical vertebra.
- The transverse cervical artery is divided into two branches: superficial and deep.
- The superficial branch runs superficially in the lateral cervical area before passing underneath the trapezius muscle (together with the accessory nerve). The deep branch divides into two smaller arteries, one of which follows the dorsal scapular nerve along the scapular medial line. The suprascapular artery runs above the scapula, behind the clavicle, and in front of the anterior scalene muscle. It joins the scapular circumflex and thoracoacromial arteries (via the acromial branches).
Muscular Region
The costocervical trunk appears behind the anterior scalene muscle and splits into two major branches:
- The supreme intercostal artery is the largest of the intercostal arteries, supplying the upper two intercostal spaces, deep neck and back muscles, back tissue, and the vertebral canal.
- As the trunk descends, it inevitably leads to the deep cervical artery, which supplies the deep neck musculature between the first rib and the seventh cervical vertebra.
Cervical Region
The deep branch of the transverse cervical artery often appears directly from the subclavian artery lateral to the anterior scalene muscle. The artery is then known as the dorsal scapular artery. It travels through the brachial plexus in this scenario, normally between the upper and middle trunks.
Clinical Points
Variant Position
If the normal embryological aortic arch formation fails, the subclavian vessels can emerge from abnormal locations.
The most familiar example is an aberrant right subclavian artery, which results in a vessel that emerges distal to the left subclavian artery and runs posteriorly between the trachea and esophagus, causing compression and breathing difficulties or dysphagia. A right aortic arch can be associated with an abnormal left subclavian artery.
Other differences occur when branching patterns are used. It is known as the accessory inferior thyroid artery if the inferior thyroid artery emerges from it rather than the natural origin of the thyrocervical trunk.
Subclavian Artery Aneurysm
This medical condition is quite rare, but its significance in modern medicine should not be overlooked. Despite the pathology’s low prevalence, it is important to understand that the disease’s course for the patient is associated with the development of serious complications that can lead to injury or even death. Complications are highly difficult to anticipate, and risk stratification for such patients is much too complex. It is also understood that the diagnosis of a subclavian artery aneurysm is often an unintentional discovery, as the disease will progress symptom-free for a long time. Around the same time, the subclavian artery ranks first in terms of the incidence of localization of upper-limb aneurysms, making this a pressing problem. Furthermore, special attention should be given to new methods of treating this disease, as the incorporation of high-tech interventions into vascular surgery has greatly increased the operating surgeon’s arsenal.
Aberrant Right Subclavian Artery
One of the most common congenital vascular defects of the aortic arch is an aberrant subclavian artery (ASCA). The majority of ASCAs are associated with an aneurysm that occurs at the descending thoracic aorta’s root, namely the Kommerell’s diverticulum.
Several surgical techniques for repairing ASCA and Kommerell’s diverticulum have been identified. Traditionally, care involved open surgery; however, recent studies show a trend away from traditional treatment and toward more hybrid or endovascular treatments. Because of the variability in the anatomy and appearance of these clinical entities, as well as patient-related variables, randomized studies for the best available modality of care have not been conducted. The latest guidelines do a good job of illustrating this lack of literature.
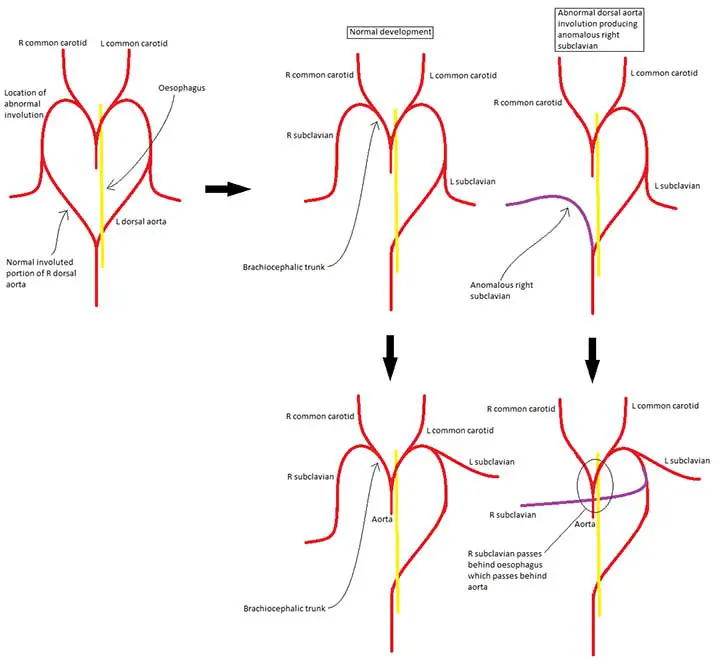
The optimal surgical technique must be customized to each patient based on their appearance, individual anatomy, and risk profile. Conventional surgery for ASCA and Kommerell’s diverticulum has a low mortality and complication rate, while hybrid repairs have shown promising results. More research is needed to provide adequate evidence to develop a consistent framework of treatment indications and optimal surgical procedures, as well as to assess long-term outcomes following hybrid repair.
Subclavian Artery Stenosis
Around 5% of patients recommended for coronary artery bypass (CABG) surgery have atherosclerotic subclavian artery disease. Because of its resilience, the internal mammary artery, a branch of the subclavian artery, is the most commonly used graft to restore coronary circulation. Stenosis or occlusion of the subclavian artery may result in retrograde blood flow in the ipsilateral internal mammary artery, compromising coronary circulation supplied by the graft. Stealing may be asymptomatic or cause symptoms of myocardial ischemia. Coronary subclavian steal syndrome post-CABG refers to symptomatic subclavian artery stenosis following bypass surgery. The occurrence is not well established, and the benefits of screening CABG patients are unknown. Despite the different methods for detecting subclavian artery stenosis, existing recommendations do not offer guidance on screening high-risk patients for this condition. Detecting subclavian artery disease before CABG will minimize the risks of post-mammary artery graft cardiac ischemia.
Subclavian Steal Syndrome
Both subclavian steal syndrome and subclavian steal phenomenon are caused by extreme proximal subclavian artery stenosis or occlusion, which causes retrograde flow in the ipsilateral vertebral artery.
The Subclavian Artery Summery
The subclavian arteries are located just below the clavicles and supply blood to the bilateral upper extremities, as well as the head and neck. The brachiocephalic trunk gives rise to the right subclavian artery, while the aortic arch gives rise to the left subclavian artery. Between the anterior and middle scalene muscles, the subclavian arteries run laterally. The subclavian artery’s distal limit is the lateral boundary of the first rib, where it merges with the axillary artery. The internal thoracic artery, vertebral artery, costocervical trunk, thyrocervical trunk, and dorsal scapular artery are all branches of the subclavian arteries. The left subclavian artery emerges from the seventh intersegmental artery during development, while the right subclavian grows in parts, proximally from the fourth aortic arch, medially from the dorsal aorta, and distally from the seventh intersegmental artery.
Last Updated on February 23, 2022 by Learn From Doctor Team