Table of Contents
Brachial Pulse Overview
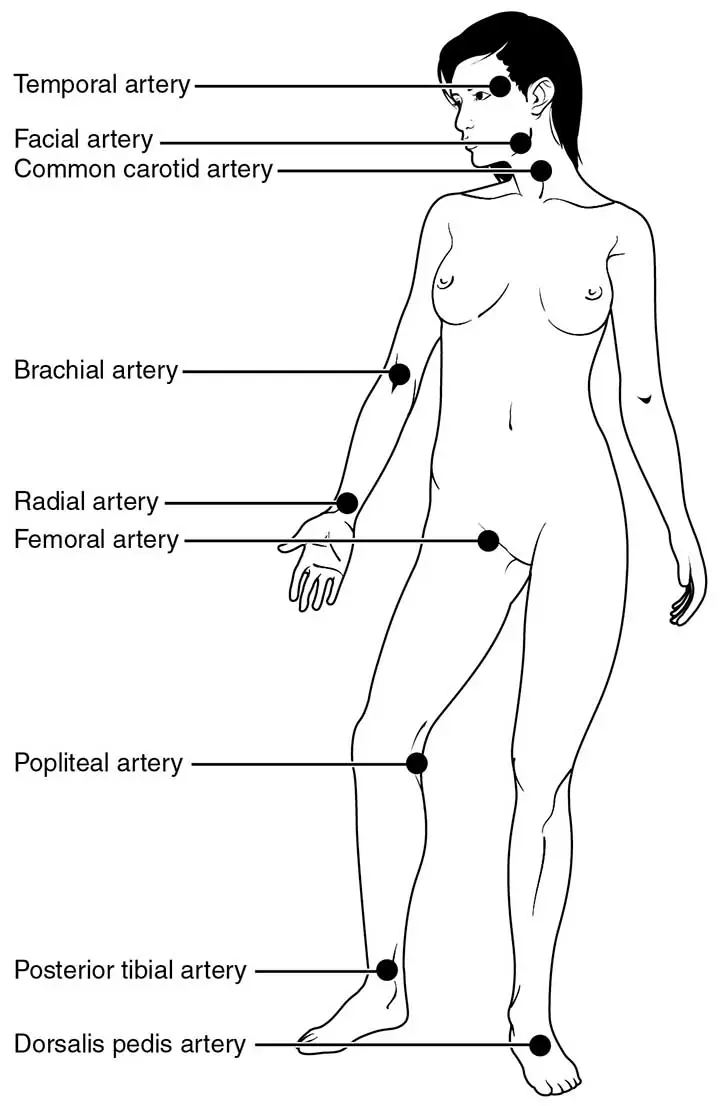
During some examinations & tests, such as those with infants, the brachial pulse rate is suggested because it can be difficult to feel the radial pulse. If necessary, a Doppler may be used to locate the brachial pulse.
Technique of Measuring
Feel the bicep tendon in the region of the antecubital fossa to find the brachial pulse. To find the pulse, shift the pads of your three fingers medially (about 2 cm) from the tendon and 2–3 cm above the antecubital fossa.
Key Points
It could assist to hyperextend the arm to accentuate the brachial pulse so you can feel it better. You may need to adjust your fingers slightly to find the best spot to reliably feel the pulse. To palpate the brachial pulse, you will normally need to push fairly firmly.

Read The Radial Artery
Measuring the Brachial Pulse in Detail
Locate the Brachial Artery. Read the anatomy of the cubital fossa if you need it.
- Extend an arm and turn it so that your inner elbow is facing up. Relax your arm and slightly extend it at the elbow. It does not have to be rigid. The crease of the elbow, also known as the cubital fossa, should be visible and easily accessible.
- Just above the cubital fossa, place your fingers on your upper arm. Feel around in the area just above the elbow crease. You can feel a small indent between your bicep and brachialis muscles, just above the inside of your elbow. These muscles can come together around the cubital fossa’s midpoint.
- If possible, use your index and middle fingers. These fingers would have the simplest time detecting the pulse. Using your index finger instead, since it has its own pulse that can throw off your readings.
- The brachial artery on your inner arm should be visible.
- To feel for a beat, keep your fingers still. The presence of a pulse means that you have located the brachial artery. The beats will be light, close to your wrist or neck pulse. Feel for your pulse on your neck if you’ve never taken one before. A pulse is usually easiest to detect here. It should be discernible on both sides of your throat. This gives you an idea of the kind of beat you should be feeling in your arm.
- If you don’t feel the rhythm, adjust your fingers. If you can’t feel your pulse, try pushing deeper into your shoulder. Since the brachial artery is deep inside the muscle, it can need some gentle pressure to be felt. If you still can’t locate the pulse, try moving your fingers around in the cubital fossa until you hear a thump.
- The pressure should be light and gentle. You’re pressing too hard if you or the person whose pulse you’re testing experiences some pain from the pressure of your fingertips.
Measuring the Brachial Pulse in Infants
- Place the baby on their back, one arm flat against their chest. The crease of the elbow should be facing up so that you can reach it without moving the boy. If possible, do this while the baby isn’t fussy or jumping around too much, so you can get the best reading.
- Feel for a beat with two fingers just above the elbow crease. Move your index and middle fingers gently around the baby’s upper arm, just above the cubital fossa, until you feel a pulse. The beat will be really light, so work slowly to avoid missing it.
- To obtain a pulse reading, gently compress your fingers. Once you believe you’ve located the brachial artery, gently compress your fingers to feel the full pulse. You should be compressing just enough to indent the baby’s skin.
- It is difficult to find an infant’s pulse. Keep distractions to a minimum and concentrate solely on the beats.
- If you’re not sure how hard to push, ask your doctor the next time you bring your baby in for a checkup. They will teach you how to test for a pulse properly.
Read The Allen’s Test
Counting the Pulse
Quick Count(15 seconds)
Multiply the 15-second pulse count by (4)four. The pulse counts how many times your heart beats in a minute. To get a full minute, multiply the number of thumps felt during your 15-second check by four. This gives you the total count of your 60-second pulse.
So, if you felt 16 beats while checking your pulse, multiply that by 4 to get a pulse rate of 64 beats per minute.
The Standard Count(60 seconds)
For the most reliable reading, check the pulse for a full 60 seconds. Taking the pulse for 15 seconds provides an accurate approximation of the overall pulse rate. Measuring the pulse for an entire 60 seconds, on the other hand, provides the most precise reading so you can sense the frequency and regularity of the beats. Count the number of beats from the brachial artery for 60 seconds using a clock, stopwatch, or timer.
Taking the brachial pulse for 60 seconds helps you to detect missed or arrhythmic beats that might not be detected in a 15-second scan. For heart patients or those in shock, a 60-second reading is recommended.
You can also get a more reliable reading by repeating the 15-second count several times and calculating the average of the readings.
It’s best to read pulse for 60 seconds.

Clinical Points
Coronary Event Indicator
The measurement of brachial pulse pressure (PP) is a well-established risk factor for cardiovascular disease. In young subjects, PP is primarily determined by stroke length, though the progressive amplification of pulse waves from central to peripheral arteries can cause brachial PP to be unrepresentative of central PP. With increasing age, brachial PP more accurately represents the gradual stiffening of the aorta and broad elastic arteries. PP is associated with vascular and cardiac hypertrophy, though the relationship with cardiac hypertrophy seems to be more closely related to systolic blood pressure (BP). Several longitudinal studies have found a connection between PP and the occurrence of major cardiovascular events. However, several long-term research of subjects with mainly systolic and diastolic hypertension found that PP is the most important predictor of coronary events, whereas mean blood pressure is the most important predictor of cerebrovascular events. In subjects with isolated systolic hypertension, a wide PP appears to predict coronary and cerebrovascular events to a similar degree. Pathophysiologically, a wide PP may indicate diffuse atherosclerotic processes that may also include the large coronary arteries. Some evidence suggests that a large PP can also be a clear and independent trigger for the development of atherosclerosis.
Contraindication of Measuring Blood Pressure(Brachial Artery)
The level of blood pressure Continuous intra-arterial monitoring via a line inserted in the radial artery is needed in critically ill patients (or the femoral in vasoconstricted patients or where access is difficult). The brachial artery should be avoided because it is a narrow end artery whose occlusion results in hand ischemia. When there is systemic vasoconstriction, mean arterial pressure (MAP) can be normal or even high, despite the fact that cardiac output is low. In contrast, if there is peripheral vasodilation, such as in sepsis, the MAP may be poor despite a high cardiac output.
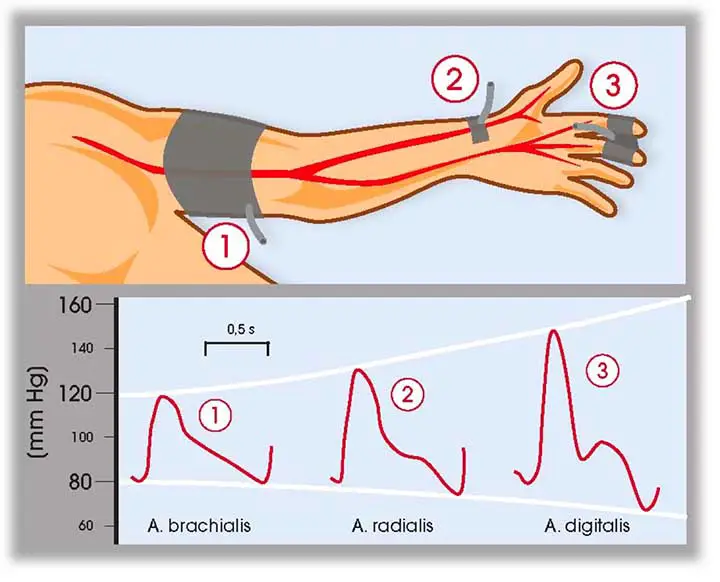
Circulation
The process of circulation In the collapsed or unconscious patient, the carotid pulse should be sought, but peripheral pulses should be tested. As the shock progresses, the brachial pulse along with the radial pulse, and femoral pulses may vanish, indicating the intensity of circulatory compromise.
Venous access for medication and/or fluid administration is critical but also difficult in ill patients. The size of the cannula required is determined by its function. Rapid fluid administration necessitates the use of wide-bore cannulae. In the extremely hypovolaemic patient, two 16G or larger cannulae should be implanted, one in each arm. If the two cannulae are different sizes, position the pulse oximeter on the same side as the larger one and the blood pressure cuff on the same side as the smaller one. This allows for unhindered volume resuscitation and continuous oxygen saturation control. For rapid, high-volume fluid resuscitation, especially blood products, pressure infusors, and blood warmers should be used. For drug administration, an 18G cannula is appropriate.
Machine-derived cuff BP measurement is unreliable at high and low blood pressures, as well as in tachycardia, especially atrial fibrillation. In hypotension, manual sphygmomanometer BP readings are more reliable. If extreme hypotension cannot be corrected with fluid alone, arterial line injection and vasoactive drug therapy should be considered as soon as possible.
Brachial Pulse in Children
Sometimes it’s hard to read the radial pulse in children. In that case, the doctors or health workers prefer the brachial pulse or popliteal pulse.
Last Updated on February 23, 2022 by Learn From Doctor Team