Table of Contents
Styloid Process Overview
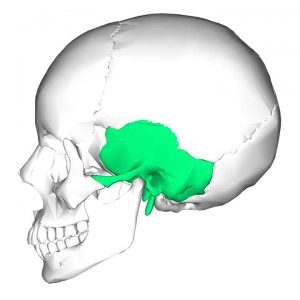
The temporal and ulnar styloid process is one of the important anatomical structures. The temporal styloid process can be found in the inferior part of the temporal bone and the ulnar styloid process can be found on the medial and posterior part of the ulna.
Temporal Styloid Process
The styloid process is characterized by a cylindrical, slender, needle-like projection with varying lengths ranging from 2 to 3 cm. The styloid process protrudes from the petrous temporal bone and connects to the stylohyoid ligament as well as the stylohyoid, stylopharyngeus, and styloglossus muscles. The styloid process enables movement of the tongue, pharynx, larynx, hyoid bone, and mandible through these structures. The styloid process is surrounded by several vessels and nerves. The internal jugular vein, internal carotid artery, the glossopharyngeal nerve (CN IX), vagus nerve (CN X), and accessory nerve (CN XI) all run through the styloid process. Along its lateral line, the occipital artery, and hypoglossal nerve (CN XII) pass. It develops from Reichert’s cartilage, which forms from the second pharyngeal arch, and undergoes endochondral ossification from the late stages of pregnancy to the first decade of life. Individuals differ in length, angulation, and other morphological features of the structure. While these physiological variations are often discovered by chance, certain patients may experience a cluster of symptoms known as Eagle syndrome. Eagle syndrome symptoms are caused by pain and/or compression of surrounding structures caused by an irregular styloid process.
Anatomical Structure and Function
The cylindrical and needle-like structure has a gradually tapering thickness that forms the styloid process’s apex. The length of the process varies from person to person, with an average length of 2 to 3 cm. While straight projection is the most common, it can vary from person to person and has been found to be curved in some individuals. The styloid process protrudes from the petrous temporal bone, inferior and anterior to the external auditory meatus, anteromedial to the mastoid process, and anterior to the stylomastoid foramen. It is made up of two parts: a proximal and a distal section. The proximal portion consists of the process’s foundation, which is located within the vaginal process of the temporal bone’s tympanic portion. The shaft is the distal part, and it is the root of three muscles: the stylohyoid, stylopharyngeus, and styloglossus. The styloid process apex is also the root of two ligaments: the stylohyoid ligament, which attaches to the hyoid’s lesser cornu, and the stylomandibular ligament, which attaches to the mandible’s ramus. Both ligaments enable the tongue, pharynx, larynx, hyoid bone, and mandible to move.

Vascular Anatomy
Several important vessels are located near the styloid process. The internal jugular vein and the internal carotid artery, as well as its branches, are located on the medial side of the styloid process, as are the lingual artery, facial artery, superficial temporal artery, and maxillary artery. The external carotid artery and one of its branches, the occipital artery, run along the lateral border of the styloid process.
Muscles and Nerves
The styloid process is responsible for the development of three muscles: the styloglossus, stylohyoid, and stylopharyngeus. The styloglossus receives innervation from CN XII, connects to the tongue’s apex, and draws up the sides of the tongue to form a conduit that aids in swallowing. The stylohyoid bone is innervated by CN VII; it connects to the greater cornu of the hyoid bone through a distal tendon perforated by the intermediate tendon of the digastric muscle and elevates the hyoid bone during swallowing. The stylopharyngeus muscle is supplied by CN IX, binds to the thyroid cartilage, and aids in laryngeal elevation as well as pharyngeal elevation and dilation during swallowing. Furthermore, on the medial aspect of the styloid process, the superior constrictor muscle and the pharyngobasilar fascia are adjacent to the tonsillar fossa.
Several nerves surround the styloid process. The glossopharyngeal nerve (CN IX), the vagus nerve (CN X), and the accessory nerve are located on the medial aspect, especially around the internal jugular vein (CN XI). The facial nerve (CN VII) and the hypoglossal nerve are located lateral to the styloid process (CN XII). The facial nerve leaves the skull through the stylomastoid foramen, which is immediately posterior to the styloid process; however, it moves laterally to the process as it pierces through the parotid gland before splitting into its subsequent branches.
Development
Reichert’s cartilage, which develops from the second pharyngeal arch during embryological development, gives rise to the styloid process. Reichert’s cartilage is divided into four sections: the tympanohyal section, the stylohyal section, the ceratohyal section, and the hypohyal section. The tympanohyal part grows antenatally, binds to the petrous portion of the temporal bone, and gives rise to the styloid process’s base, which is ensheathed by the tympanic part’s vaginal process. The stylohyal part develops after birth and gives rise to the shaft of the styloid process as well as the proximal portion of the stylohyoid ligament. After puberty, the stylohyal part may or may not merge with the tympanohyal part; in some cases, they never do. The ceratohyal and its fibrous sheath regress, resulting in the formation of the stylohyoid ligament. The hypohyal portion gives rise to the hyoid bone’s lesser cornu.
The styloid phase is characterized by endochondral ossification, which starts in the final stages of pregnancy and continues for the first 8 years of life. However, the ossification pattern and time to complete ossification have been shown to differ greatly.
Variation in People
The length of the styloid process varies between individuals, with research showing average lengths ranging from 1.52 cm to 8 cm. Within the same individual, the lengths of the left and right styloid processes can differ. Although the length of the styloid process varies from person to person, anything longer than 3 cm is considered elongated. An elongated styloid process is estimated to affect approximately 4% of the general population. However, there are significant differences between groups, with rural Indian populations showing a much higher prevalence.
An elongated styloid process is more common in women than in men.
Variation can also be seen in the styloid process’s ossification and fusion. As previously stated, the stylohyal component can merge with the tympanohyal after puberty. If the stylohyal component successfully fuses with the tympanohyal component and the stylohyal element ossifies, the styloid process is prolonged. However, if the stylohyal portion fails to ossify, the styloid process is shortened.
Several hypotheses have been suggested to explain the variation in ossification and elongation of the styloid process’s etiology. The first hypothesis is the “theory of reactive hyperplasia,” which argues that after pharyngeal trauma, the styloid mechanism responds and proliferates, causing elongation. The second theory, the “theory of reactive metaplasia,” is similar to the first in that trauma is the initiating factor. However, the second hypothesis proposes that the stylohyoid ligament, which undergoes metaplasia and partial ossification, is the mechanism responsible for the irregular ossification. The third theory is the “theory of anatomic variance,” which proposes that the ossification of the styloid process and the stylohyoid ligament is a natural process reflecting an anatomical variation that results in styloid process elongation. A fourth hypothesis proposes that the elongated styloid process is caused by preserved embryologic tissue from Reichert’s cartilage. While these hypotheses provide potential explanations for the variations observed in the styloid phase, no consensus has been reached.
Clinical Points
Eagle Syndrome
An elongated styloid process affects about 4% of the general population. While the vast majority of these people are asymptomatic, a small percentage of those with an elongated styloid process do experience symptoms and may have either of two forms of Eagle syndrome. The classic Eagle syndrome, also known as stylohyoid syndrome, manifests as a sharp pain in the neck or ear that spreads to the maxilla, face, and oral cavity. With head rotation, chewing, swallowing, stretching the tongue, or yawning, the pain can appear exaggerated. It can also be associated with a pharyngeal foreign body sensation, tinnitus, or vertigo. A mass can also be palpable in the tonsillar fossa. Symptoms of classic Eagle syndrome are typically unilateral, but they can appear bilaterally in rare cases. These symptoms are caused by inflammation or potential entrapment of adjacent cranial nerves (CN V, VII, IX, or X). It is normal to see classic Eagle syndrome after a tonsillectomy or other pharyngeal surgery. The discomfort or entrapment that occurs may be a result of the formation of local granular cells.
The stylocarotid artery syndrome is the second form of Eagle syndrome, which arises when the styloid process impinges on the internal or external carotid artery and the nerve plexus that surrounds them. It manifests as pharyngeal pain, eye pain, or parietal cephalgia, which is similar to a migraine or a cluster headache. Internal carotid artery compression may cause symptoms of internal carotid vascular insufficiency such as fatigue, visual changes, or syncope that is aggravated by head movement. The elongated styloid process can also increase the risk of carotid artery dissection, which could result in a transient ischemic attack or stroke.
So far, studies examining the potential relationship between the duration of the styloid process and the severity of symptoms have been inconclusive. Correlations between angulation, duration of the styloid process, and overall development of Eagle syndrome, on the other hand, have been suggested. If the styloid process deviates laterally, it will almost certainly come into contact with the external carotid artery and its branches. If the styloid process deviates laterally, it can impinge on CN IX, CN X, CN XI, and CN XII, which are located between it and the atlas’s transverse process. Furthermore, if the styloid process deviates medially or anteriorly, it can irritate the tonsillar fossa and the essential structures it contains.
Diagnosis
Eagle syndrome is diagnosed based on the patient’s clinical presentation, radiological examination, and lidocaine infiltration test. Eagle syndrome has a non-specific clinical appearance that can be confused with a number of other diagnoses. A palpable mass in the tonsillar fossa can help the clinician narrow the differential diagnosis; although, it is not always present in symptomatic Eagle syndrome. A lateral head and neck X-ray may detect the elongated styloid process, but bilateral processes can overlap and misdirect the diagnosis. A Towne radiograph, which is an anterior-posterior skull axis view, may be used to measure styloid process medial or lateral deviation. The styloid process’s size and angulation can be measured using computed tomography (CT). A 3D-CT is the gold standard in radiological diagnosis and is the perfect supplement to a standard X-ray. To evaluate blood flow patterns in stylocarotid syndrome, CT angiography is suggested. For symptomatic patients, the lidocaine penetration test may be used to confirm the diagnosis. If 1 ml of 2 percent lidocaine is applied to the region surrounding the palpable styloid process and the patient’s symptoms are reduced, the test is deemed positive and the diagnosis of Eagle syndrome is established.
Treatment
Depending on the seriousness of the condition, Eagle syndrome may be treated conservatively or surgically. However, cautious management is advised at first. For symptomatic relief, steroid or long-acting anesthetic injections at the inferior portion of the tonsillar fossa or the lesser cornu of the hyoid bone are used. An extra-oral transcervical approach or an intra-oral transpharyngeal approach may be used for surgical management. The extra-oral transcervical technique improves visualization but is more complex and time-consuming, leaving a noticeable scar and possibly temporary weakness in the marginal mandibular nerve. The intra-oral method reduces operating time and allows for the use of a local anesthetic; however, poorer visualization presents a risk to the main vessels of the neck, as well as an increased risk of bacterial infection. External manipulation and fracturing of the elongated styloid process under local anesthesia have been suggested, but long-term findings have been unsatisfactory.
Summary of Temporal Styloid Process
The temporal bone’s styloid process is a slender osseous projection that protrudes anteroinferior from the inferior surface of the petrous portion of the temporal bone.
It is the anchor point of several muscles and ligaments. These are;
- The styloglossus muscle
- The stylohyoid muscle
- The stylopharyngeus muscle
- The stylohyoid ligament
- The stylomandibular ligament
Variations
- Normal (less than 30 mm)
- Elongated (more than 30 mm)
- Pseudoarticulated
- Segmented
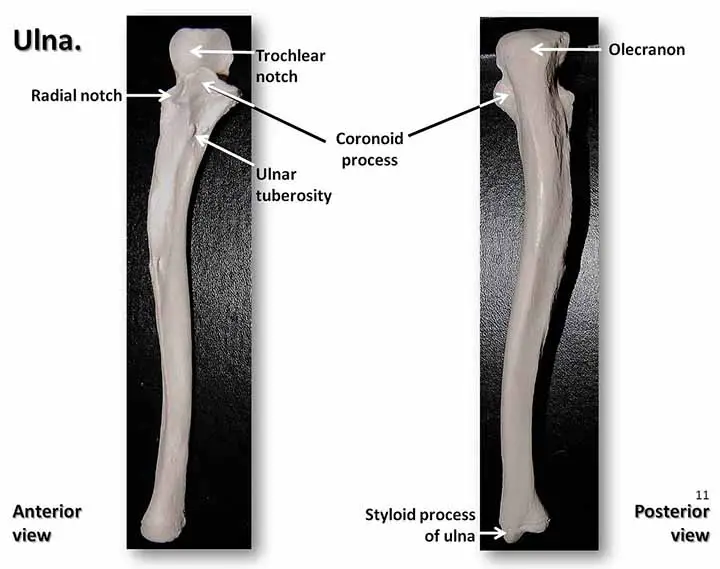
Ulnar Styloid Process
The ulna’s styloid process projects from the medial and posterior ulna. It falls slightly lower than the head. Depression for the attachment of the apex of the triangular articular disk and a shallow groove for the tendon of the extensor carpi ulnaris muscle distinguish the head from the styloid process.
The ulnar styloid process ranges in length from 2 to 6 mm.
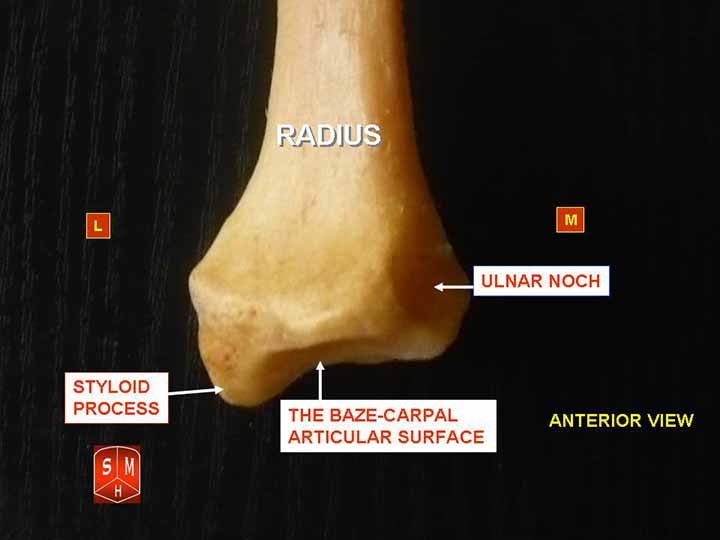
Attachments
The rounded end of the ulna’s styloid process connects to;
- The ulnar collateral ligament of the wrist.
- The radioulnar ligaments to the base of the styloid process.
Read The Ulnar Artery
Clinical Points
Ulnar Styloid Fracture
The key symptom of an ulnar styloid fracture, as with any other form of fracture, is acute pain. This form of fracture is often associated with a radius fracture. If this occurs, you will most likely experience pain on the inside of your wrist rather than near the ulnar styloid process.
Some associated Symptoms
- Redness
- Swelling
- Tenderness
Causes
- Road traffic accidents
- Bike accident
- Fall on hands
- Certain sports injuries
Treatment
Non-Surgical
Mild ulnar styloid fractures are mostly treated with a simple wrist cast. Your doctor may need to realign bones before applying a cast in certain situations. This is known as reduction, and it can often be performed without an incision (closed reduction).
Surgical Procedure
More serious fractures, including those affecting other adjacent bones, would almost certainly necessitate surgery. An open reduction is used in this case: the doctor will make an incision near the break and use the opening to reset the affected bones. Severe fractures can necessitate the use of metal screws or pins to hold the bones in place until they heal.
Read Seizure Precaution Nursing
Few Last Words
The styloid process is an essential anatomical divider of the para-pharyngeal space (PPS). The tensor-vascular-styloid fascia divides the body into distinct compartments. From the styloid process to the tensor veli palatini muscle, this fascia runs. To aid in the differential diagnosis of PPS lesions, the PPS is divided into prestyloid (anterolateral) and retrostyloid (posteromedial) compartments. Fat, a portion of the retromandibular parotid gland, and lymph nodes are all included in the prestyloid compartment. The internal carotid artery, internal jugular vein, CN IX-XII, a part of the sympathetic chain, and lymph nodes are all found in the retrostyloid zone. However, it has been suggested that this form of PPS compartmentalization does not have the best surgical solution.
Last Updated on February 23, 2022 by Learn From Doctor Team