Table of Contents
Tibial Nerve Overview
The tibial nerve is a major lower-limb peripheral nerve. It performs a variety of cutaneous and motor functions in the leg and foot. The tibial nerve compression can cause tarsal tunnel syndrome.
Root Value of Tibial Nerve
Ventral division of ventral rami of L4, L5, S1, S2, S3.
Course
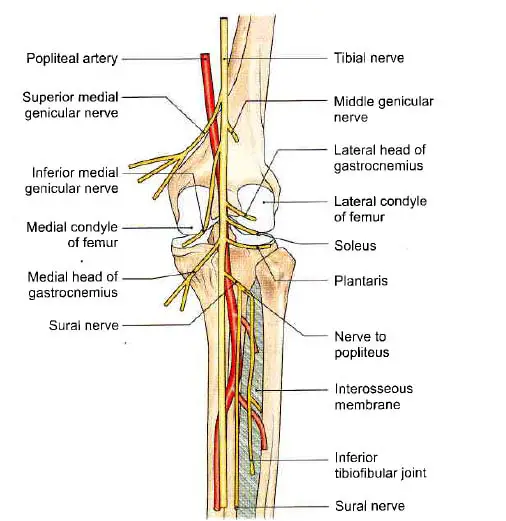
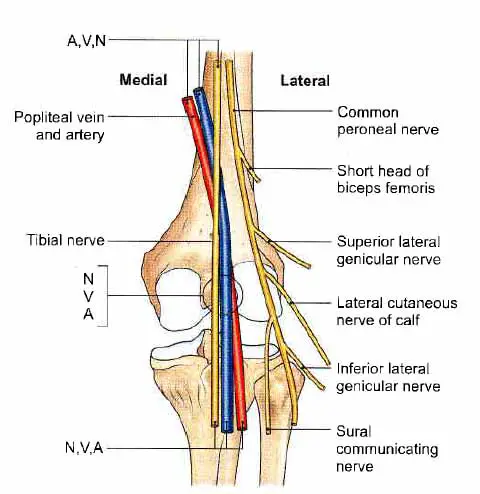
This is the larger sciatic nerve terminal branch. It is located either superficially or posteriorly to the popliteal vessels. It runs from the superior angle of the popliteal fossa to the inferior angle, passing the popliteal vessels from lateral to medial.
Read Popliteal Artery
Branches
- In the upper part of the fossa, three genicular or articular branches appear:
- The superior medial genicular nerve is located deep inside the muscles, above the medial condyle of the femur.
- The middle genicular nerve pierces the posterior part of the knee capsule to supply structures in the femoral intercondylar notch.
- The inferior medial genicular nerve runs along the upper border of the popliteus and goes down to the medial condyle of the tibia.
- Sural is the name given to the cutaneous nerve, which originates in the middle of the fossa and escapes at the inferior angle. It supplies on the lower half of the back of the leg as well as the entire lateral border of the foot until the tip of the little toe.
- Muscular branches for the lateral and medial heads of the gastrocnemius, soleus, plantaris, and popliteus appear in the distal part of the fossa.
The popliteal nerve crosses the popliteal artery, passes downward and laterally, winds along the popliteus’ lower border, and supplies it from its deep (anterior) surface. The nerve also supplies the tibialis posterior, the superior tibiofibular joint, the tibia, the interosseous membrane, and the inferior tibiofibular joint, in addition to the popliteus.
Read Common, Superficial, and Deep Peroneal Nerve
Functions
Motor Functions
Leg(Posterior Compartment)
The muscles of the posterior compartment of the leg are divided into two compartments: superficial and deep. The tibial nerve innervates both of them.
Superficial
The Plantaris Muscle: Plantarflexion of the ankle.
The Soleus Muscle: Plantarflexion of the ankle.
The Gastrocnemius Muscle: Flexion of the knee and plantarflexion of the ankle.
Deep
The Popliteus Muscle: Unlocks the locked knee by laterally rotating the femur on the tibia.
The Flexor Hallucis Longus Muscle: Flexion of the great toe and plantarflexion of the ankle
The Flexor Digitorum Longus: Flexion of digits 2-5 and plantarflexion of the ankle.
The Tibialis Posterior: Inversion of the foot and plantarflexion of the ankle.
Read Popliteal Vein
Foot(Intrinsic Muscles)
The tibial nerve’s medial and lateral plantar branches innervate all of the intrinsic muscles of the foot (except the extensor digitorum brevis, which is innervated by the deep fibular nerve).
Sensory Functions
The tibial nerve has cutaneous branches in the popliteal fossa. The sural nerve is formed by combining these with branches from the common fibular nerve. The skin on the posterolateral side of the leg and the lateral side of the foot are innervated by this sensory nerve.
The foot is supplied by 3 branches of the tibial nerve
- Medial calcaneal branches
- Medial plantar nerve
- Lateral plantar nerve
Clinical Anatomy
- However, for the medial head of the gastrocnemius, the majority of the tibial nerve’s muscular branches originate from its lateral side. As a result, the medial side of the nerve is unaffected.
- Tibial nerve damage results in motor and sensory loss.
- Motor loss in the calf’s superficial and deep muscles, as well as the intrinsic muscles of the sole.
- Sensory loss: Loss of feeling in the sole, including the plantar part of the digits and the nail beds on the dorsum of the foot.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, also known as tibial nerve dysfunction or posterior tibial nerve neuralgia, is an entrapment neuropathy caused by the compression of structures inside the tarsal tunnel.
It is related to, but much less common than, carpal tunnel syndrome of the wrists.
The tarsal tunnel is a small fibro-osseous area that runs behind and under the medial malleolus. It is bounded anterosuperiorly by the medial malleolus, laterally by the posterior talus and calcaneus, and anterosuperiorly by the flexor retinaculum, which stretches from the medial malleolus to the medial calcaneus and prevents medial displacement of its components.
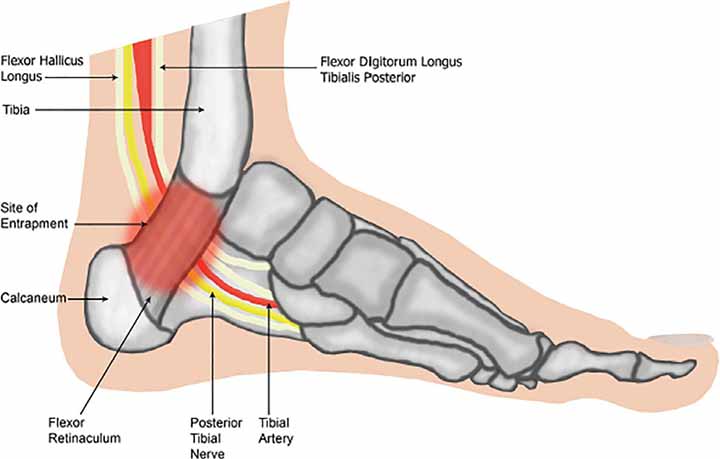
The tarsal tunnel contains a number of essential structures. It houses the posterior tibialis, flexor digitorum longus (FDL), and flexor hallucis longus (FHL) tendons. It also houses the posterior tibial artery and vein, as well as the posterior tibial nerve (L4-S3). It’s worth noting how these structures are oriented inside the tarsal tube. The tibialis posterior tendon, FDL tendon, posterior tibial artery and vein, posterior tibial nerve, and FHL tendon are located from medial to lateral.
The posterior tibial nerve runs between the FDL and FHL muscles before splitting into the medial and lateral plantar nerves in the tarsal tunnel. The bifurcation occurs before the tarsal tunnel in 5% of individuals. The medial plantar nerve supplies sensation to the medial half of the foot and the first 3.5 digits as well as motor activity to the lumbricals, abductor hallucis, flexor digitorum brevis, and flexor hallucis brevis. The lateral plantar nerve runs directly through the belly of the abductor hallucis muscle and provides sensory innervation to the medial calcaneus and lateral foot, as well as motor control to the flexor digitorum brevis, quadratus Plantae, and abductor digiti minimi. The medial calcaneal nerve normally branches off the posterior tibial nerve proximal to the tarsal tunnel and innervates the posteromedial heel. It branches off the lateral plantar nerve or runs superficial to the flexor retinaculum in 25% of patients.
Read Popliteal Fossa
Symptoms
- Continuous pain or pain with movement
- Burning type of pain
- Sensory disturbance
- Tinel sign
- Muscular atrophy or weakness
Treatment
The management of tarsal tunnel syndrome remains difficult due to diagnostic complexity and a lack of clarification about which patients will benefit from conservative versus surgical treatment. Tarsal tunnel syndrome may be treated nonsurgically or surgically. The etiology of the condition, the degree of loss of function of the foot and ankle, and muscle atrophy all play a role in this decision.
The etiology of tarsal tunnel syndrome influences conservative management and performance. The objective is to reduce discomfort, inflammation, and tissue tension. It is possible to use ice. Oral analgesics such as acetaminophen and nonsteroidal anti-inflammatory drugs (NSAIDs) may be beneficial. Gabapentin, pregabalin, and tricyclic antidepressants are examples of neuropathic pain drugs that can be attempted. Topical drugs such as lidocaine and NSAIDs may also be used.
Ultrasound, iontophoresis, phonophoresis, and E-stim are examples of physical therapy soft tissue modalities that can be beneficial. Calf stretching and nerve mobility, also known as nerve gliding, may help to reduce symptoms. Strengthening the tibialis posterior may be beneficial. Changing one’s activity level can also help with symptom management. Kinesiology tape can be used to protect the arch and reduce biomechanical tension.
Orthotic shoes can be used to remedy biomechanical issues and relieve tarsal tunnel syndrome. By inverting the heel, a medial heel wedge or heel seat can reduce traction on the nerve. Night splints can be used, and patients who do not respond to the above therapies can be temporarily put in a walking boot. Footwear with adequate arch support can help alleviate symptoms. You might try a CAM (controlled, ankle, motion) walker or walking boots.
A ganglion cyst may be aspirated under ultrasound guidance if one is present. Injections of corticosteroids into the tarsal tunnel can help with edema.
If conservative treatment fails to relieve the patient’s symptoms or a conclusive cause of entrapment is found, surgery is recommended. Patients suffering from symptoms induced by a space-occupying lesion usually respond well to surgical treatment. Nerve conduction through the posterior tibial nerve that is abnormally sluggish is indicative of unsuccessful conservative therapy.
The flexor retinaculum is released surgically from its proximal attachment near the medial malleolus down to the sustentaculum tali. Surgical success rates range from 44% to 96 percent. Patients who have a positive Tinel sign before surgery have a stronger response to surgical decompression than those who do not. Younger patients and those with a limited history of symptoms, an early diagnosis, a simple etiology, and no prior ankle pathology are more likely to respond to surgery.
Summary of Tibial Nerve
Root Value
Ventral division of ventral rami of L4, L5, S1, S2, S3, segments of the spinal cord.
Beginning
It starts as a wider division of the sciatic nerve in the back of the thigh.
Course
The tibial nerve’s path and relationships in the leg are close to those of the posterior tibial artery. The tibial nerve, like the artery, terminates by splitting into the medial and lateral plantar nerves.
In the popliteal fossa: From its upper angle to its lower angle, the nerve descends vertically in the popliteal fossa. It is next to the popliteal vessels. It extends beyond the distal border of the popliteus muscle in the back of the leg.
In the back of the leg: The nerve descends as the neurovascular bundle, which is connected to the posterior tibial vessels. It is located superficially to the tibialis posterior and deeply to the flexor digitorum longus. Finally, it travels deep into the ankle’s flexor retinaculum.
Branches of the Tibial Nerve
Muscular
- The tibialis posterior,
- The flexor digitorum longus;
- The flexor hallucis longus,
- The deep part of the soleus.
Cutaneous
Medial calcanean branches pierce the flexor retinaculum and supply the skin on the back and lower surface of the heel.
Articular
To the ankle joint.
Terminal Branches of the Tibial Nerve
- Medial plantar
- lateral plantar nerves
Last Updated on February 23, 2022 by Learn From Doctor Team