Table of Contents
Anatomical Overview
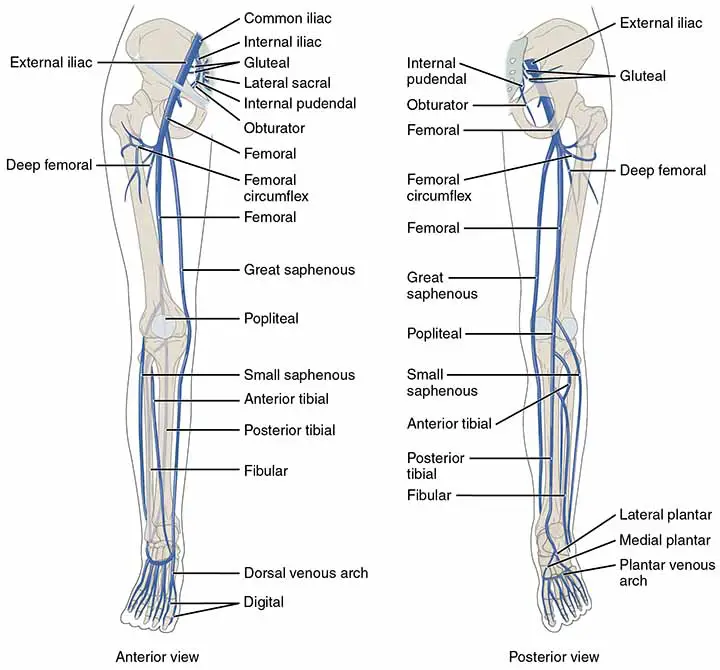
The popliteal vein starts at the lower border of the popliteus, where veins accompanying the anterior and posterior tibial arteries join. It runs medial to the popliteal artery in the lower fossa, posterior to it in the center, and posterolateral to it in the upper fossa. At the opening in the adductor Magnus, the vein continues as the femoral vein. The popliteal vein receives blood from;
- The small saphenous vein.
- The veins corresponding to the branches of the popliteal artery.
Read Anatomy of Popliteal Fossa before reading the anatomy of popliteal vein for better understanding.
Detailed Anatomy of Popliteal Vein
The popliteal vein originates from the posterior and anterior tibial veins and rises through the popliteal fossa to the gap in the Adductor Magnus alongside the popliteal artery, where it merges with the femoral vein.
As the vein ascends, its connection to the popliteal artery varies, but it is still between the popliteal artery and the tibial nerve. It is medial to the artery distally, superficial (posterior) to it between the heads of the gastrocnemius, and posterolateral to the artery proximal(close) to the knee joint.
Read Popliteal Artery
Tributaries
- The small saphenous vein(also known as the short saphenous vein) in the lower part of the popliteal fossa veins corresponding to popliteal artery branches, namely the genicular arteries
- The muscular veins, including a broad branch from each gastrocnemius muscle head
Location
The popliteal vein then rises and passes through the adductor hiatus (a gap created between the two insertions of the adductor Magnus’s muscle) to become the femoral vein, which runs superiorly and medial to the femoral artery, which is itself medial to the femoral nerve. The femoral nerve passes under the inguinal ligament and innervates the anterior compartment of the thigh.
Clinical Anatomy
Popliteal vein aneurysm
Popliteal vein aneurysms are uncommon and seldom present clinically. Surgical repair is recommended if the condition is causing symptoms such as;
- Deep Venous Thrombosis
- Pulmonary Embolism
Clinical Manifestations of Popliteal Vein Aneurysm
- Usually asymptomatic,
- It is discovered when sequelae such as DVT or PE build resistance in the popliteal fossa
- Resulting in occasional claudication.
Causes
The pathogenesis is currently unknown; congenital venous wall weakness, inflammation, trauma, and hemodynamic changes have all been proposed as causative factors. Some studies are going on, hope we’ll know about that when those studies bring up the result.
Diagnosis
Phlebography: It used to be the gold standard, but it is no longer widely used.
Ultrasound: The initial imaging modality of choice, responsive, with color Doppler, also allows for dynamic blood flow assessment.
CT: CT and MRI angiography may also be used to demonstrate pathology.
Read Peroneal Nerve
Treatment
Open surgical treatment is mostly used for it.
Differential Diagnosis
- Popliteal artery aneurysm
- A popliteal cyst (also known as Baker’s cyst)
- Cyst around the synovial sarcoma
Complication
- Deep Vein Thrombosis
- Pulmonary Embolism
Deep Vein Thrombosis
Deep vein thrombosis (DVT) is most common and generally occurs in lower limbs, but it can also occur in the upper limb and neck veins. Other forms of venous thrombosis, such as intraabdominal and intracranial thrombosis.
Causes of DVT
The cause of DVT is most likely multifactorial, immobility (and thus stasis) is one of the most significant factors. DVT is recognized as a complication of long-distance flights and other modes of transportation.
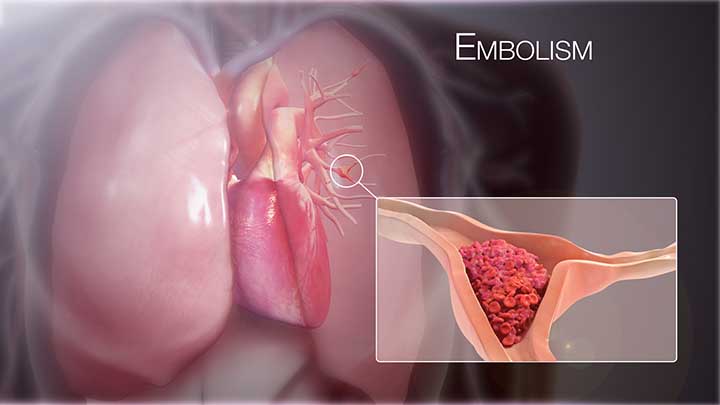
A platelet aggregate forms the basis of the thrombus. Fibrin and red cells then form a mesh, occluding the lumen of the vein wall. The coralline thrombus then develops into a propagated loose red fibrin clot with numerous red cells. This is likely to spread to the next broad venous branch, and the clot will break off and embolize to the lung as a pulmonary embolus. In this case, an embolus form in the lower leg veins, travels through the vast veins of the limb and vena cava, through the right heart, and lodges in the pulmonary arteries. This can completely obstruct perfusion to all or a portion of one or both lungs. This results in a clinical continuum ranging from tachycardia and discomfort to respiratory failure (despite proper ventilation) and death.
On imaging, moderate-sized emboli can cause pyramidal-shaped infarcts.

Diagnosis of Deep Vein Thrombosis (DVT)
The most common symptom of a DVT is pain and swelling, especially in the calf, typically in one leg; however, bilateral DVTs are common, support for approximately 30% of all cases. DVT must be distinguished from other causes of systemic Oedema, such as hypoproteinaemia, renal failure, and heart failure, especially when the swelling is bilateral. Some patients have no thrombotic symptoms and can initially present with signs of a pulmonary embolus, such as pleuritic chest pain, hemoptysis, and difficulty in breathing. Chronic pulmonary hypertension can also cause shortness of breath in patients. Phlegmasia alba dolens and phlegmasia cerulea dolens both have cellulitic legs that are occasionally white or cyanosed. This means that venous pressures are so high that tissue perfusion is being hampered. Patients with venous gangrene often have an underlying neoplasm.
Dorsiflexion – this is not a particular movement and should not be garnered. Tenderness is present in 75% of patients, but it is also present in 50% of patients who do not have clinically confirmed DVT. The size, place, or extent of the thrombus does not normally correlate with the pain and tenderness associated with DVT. Around 10% of patients with reported DVT have clinical signs and symptoms of pulmonary embolus.
Low-grade pyrexia may be present, especially in patients with recurrent pulmonary embolus. If a patient has pulmonary emboli causing right heart pressure, they may show signs of cyanosis, dyspnea, raised neck veins, a fixed split-second heart sound, and a pleural rub, but these signs may be subtle or missing.
Read The Tibial Nerve
Investigations
- Ultrasound
- MRI
Treatment Procedure
The best treatment for DVT is anticoagulation. Sometimes it takes more than 8-12 weeks.
Complications
- Pulmonary Embolism
- Vein(Venous) Thromboembolism
- Phlegmasia cerulea dolens
- Post-thrombotic syndrome
Pulmonary Embolism
A pulmonary embolism is a blockage of one or more arteries of the lung. Most pulmonary embolisms are caused by blood clots that migrate to the lungs from deep veins in the legs or, in some extremely rare cases, veins in other parts of the body (deep venous thrombosis).
Pulmonary embolism can be life-threatening because the clots block the blood supply to the lungs. However, timely care decreases the risk of death significantly. Preventing blood clots in your legs will help protect you from pulmonary embolism.
Signs and Symptoms
- Difficulty in breathing
- Chest pain
- Sometimes severe coughing
Complications
Pulmonary embolism is a potentially fatal condition. One-third of people who have undiagnosed and untreated pulmonary embolism die. However, when the disease is diagnosed and treated promptly, the figure drops significantly.
Pulmonary embolism may also result in pulmonary hypertension, a condition in which the blood pressure in your lungs and right side of your heart is abnormally high. When the arteries within your lungs become clogged, your heart has to work harder to pump blood into those veins, increasing blood pressure and gradually weakening your heart.
Small emboli are common in rare cases and gradually develop over time, resulting in chronic pulmonary hypertension(also known as chronic thromboembolic pulmonary hypertension).
Treatment
Most of the time anticoagulation. Sometimes if the condition is severe then surgical procedure.
Last Few Words
The popliteal vein is one of the important veins of the lower limb. From it can arise complicated medical conditions such as DVT and pulmonary embolism.
Last Updated on February 23, 2022 by Learn From Doctor Team