Table of Contents
Traumatic Pneumothorax
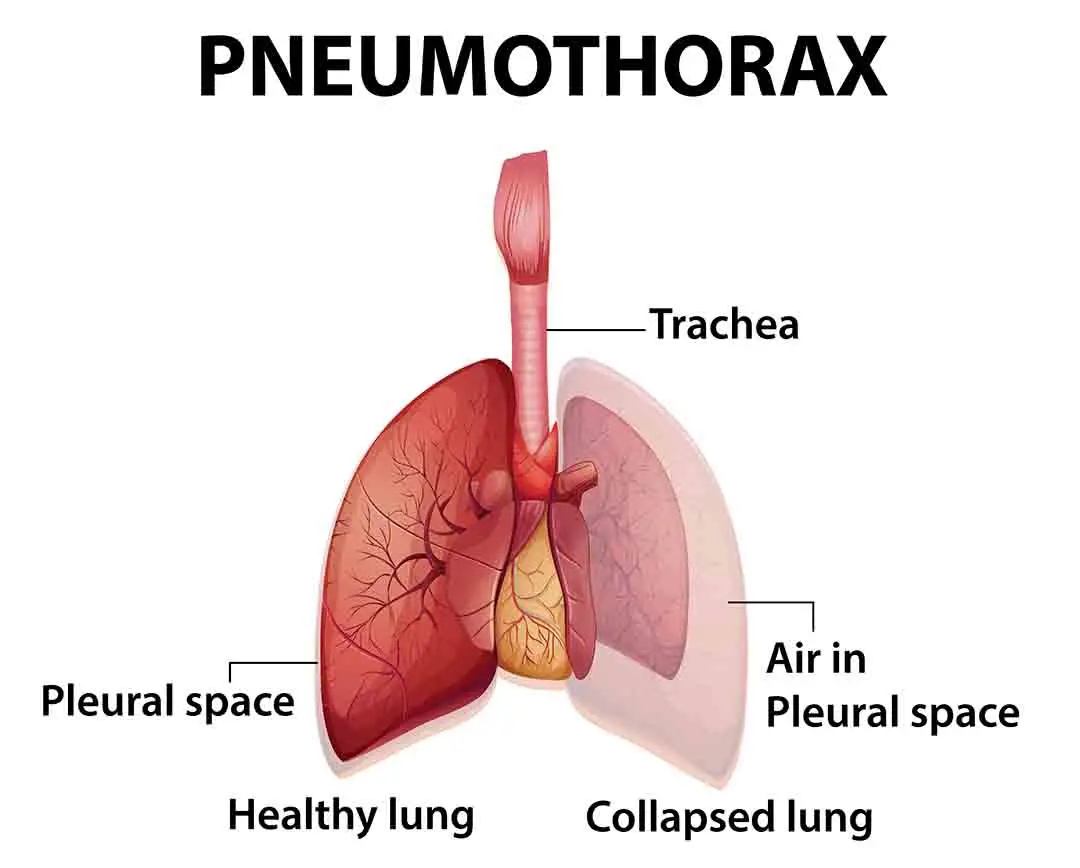
Penetrating or nonpenetrating chest trauma (injury) may cause a traumatic pneumothorax. The wound allows air to reach the pleural space through the chest wall or through the visceral pleura from the tracheobronchial tree in penetrating chest trauma.
A pneumothorax may result from non-penetrating trauma if the visceral pleura is lacerated as a result of a rib fracture or dislocation. Sudden chest compression boosts alveolar pressure rapidly, possibly causing alveolar rupture. Air reaches the interstitial space after the alveolus ruptures and dissects toward the visceral pleura or the mediastinum. When either the visceral or mediastinal pleura ruptures, air enters the pleural cavity, causing a pneumothorax.
Read Tension Pneumothorax
Mechanism of Traumatic Pneumothorax
Traumatic
- Penetrating Trauma (Injury): (such as stab wounds, bullet wounds, and impalement on a foreign body) usually injures the peripheral lung, resulting in hemothorax and pneumothorax in over 80% of all penetrating chest wounds.
- Blunt Trauma(Injury): A rib fracture, increased intrathoracic strain, and bronchial rupture may all result from blunt trauma. The “Fallen lung sign” (ptotic lung sign) occurs when the hilum of the lung is below the expected amount inside the chest cavity, or when there is a recurrent pneumothorax with a working chest tube.
Read Pulmonary Contusion (Lung Contusion)
Pulmonary Barotraumas
Although the volume of a given mass of gas(air) at a constant temperature is inversely proportional to its pressure, a given volume of gas(air) saturated at body temperature can increase to 1.5 times the volume at sea level if it is put at an altitude of 3050 m, resulting in a pneumothorax, as seen in aircrew members. Similar to scuba divers, compressed air is delivered to the lungs through demand regulators, and barotraumas can occur during ascent as atmospheric pressure falls rapidly, causing gas in the lungs to expand and cause pneumothorax.
Iatrogenic Pneumothorax
Causes of Iatrogenic Pneumothorax are as follows;
- Biopsy(Transthoracic needle aspiration) – Most common, around 24% of iatrogenic pneumothorax is caused by it.
- Subclavian or Jugular vein catheterization
- Pleural Biopsy(Closed)
- Thoracentesis
- Mechanical Ventilation
- Cardiopulmonary resuscitation
- Nasogastric tube placement
- Transbronchial biopsy
- Tracheostomy
- Liver biopsy
Some less common causes of iatrogenic pneumothorax
- Thoracic spine fracture with significant displacement
- In recent decades, acupuncture has been linked to pneumothorax.
- In the case studies, colonoscopy and gastroscopy have been involved.
- Intravenous drug users who prefer neck veins are more likely to be affected
Transthoracic needle aspiration is the most common cause of iatrogenic pneumothorax. It may be due to two factors: the depth and scale of the lesion. The risk of traumatic pneumothorax raises as the lesion grows deeper and narrower.
Because of the rising number of patients needing intensive care, central cannulation is the second most common cause of iatrogenic pneumothorax.
A relatively common complication of the subclavian vein puncture is an inadvertent subclavian arterial puncture. The overall reported incidence is in the range of 1-13% with 2-5% being typical. If several attempts are made, the chance of incident rises to about 40%.
The third most common cause of iatrogenic pneumothorax is thoracentesis. If performed under ultrasound control, this can be minimized. Iatrogenic pneumothorax was found to be 13 percent for computed tomography (CT)-directed transthoracic fine-needle aspiration (TFNA), 7.1 percent for pleural biopsy, 16.6 percent for transbronchial biopsy, 7.1 percent for fluoroscopy-guided TFNA, and 1.5 percent for thoracentesis in a sample of 418 invasive procedures.
Since newer ventilatory modes allow for significantly lower pressures and lower mean airway pressures, the risk of pneumothorax from mechanical ventilation has decreased. Transpleural and transbronchial lung biopsies, cardiopulmonary resuscitation, thoracic acupuncture, and intravenous substance abusers utilizing neck veins are all potential triggers.
Clinical Manifestations of Iatrogenic Pneumothorax
| Findings | Causes |
| Tachycardia and hypotension with sudden onset | Tension pneumothorax due to impending venous return |
| Increased peak airway pressure | Lung compression(external) |
| Sudden Decline in oxygen saturation(It can be mistaken with Covid-19 symptoms) | The collapse of the lung(one or both) |
| Distressed Patient | Ventilator |
Diagnosis of Traumatic Pneumothorax
Pneumothorax is diagnosed by a detailed clinical review and investigations. However, accurately diagnosing and managing the condition requires a clinical understanding of the presenting signs and symptoms.
Early Signs and Symptoms of Pneumothorax
- Chest pain with sudden onset
- Feeling tightness around the chest
- Breathlessness(shortness of breath)
- Fast heart rate(Pulse)
- Rapid Breathing(trying hard to breathe sometimes)
- Coughing
- Fatigue
- Cyanosis
Late findings are following
- Level of Consciousness decreases
- Tracheal deviation in the opposite direction
- Hypotension(sometimes severe)
- Veins in the neck are dilated (may not be present if hypotension is severe)
- Cyanosis
Radiological Studies of Traumatic Pneumothorax
In certain cases, radiological confirmation and localization of tension pneumothorax may be preferred to exposing the patient to the possible morbidities of decompression. This concern should be restricted to patients who are conscious, stable, and not in advanced stages of tension, as well as those who can obtain an immediate chest film and have the ability to perform emergency decompression if necessary.
To find out pneumothorax, serial chest radiographs every 6 hours on the first day after trauma(injury) are preferable, but two or three chest X-rays every 4-6 hours will work.
A tension pneumothorax is indicated by air in the pleural cavity and contralateral deviation of mediastinal structures. Increased thoracic length, increased rib separation, ipsilateral flattening of the heart border, contralateral mediastinal deviation, and mid-diaphragmatic depression are all possible x-ray film observations(findings).
A pneumothorax can be hidden by rotation, which can be mistaken for a mediastinal turn.
Initial observations of pneumothorax scale on a chest radiograph may be deceiving. A 2.5-cm margin of air peripheral to the collapsing lung corresponds to a pneumothorax of around 30% on the chest x-ray, which may help determine the extent of the pneumothorax. A pneumothorax is characterized as a complete collapse of the lung.
AP films of the supine chest are notoriously unreliable. Supine films often look fine, even though there is substantial air since they allow air to spread out over the anterior chest. The “deep sulcus sign,” named after the presence of a particularly deep costovertebral sulcus, is often the only indicator.
In rare cases of bilateral pneumothorax, the patient may present with extreme respiratory distress and an engorged neck vein; however, there may be no symptoms of mediastinal change, and findings on both sides of the lung would be identical.





Treatment Procedure of Traumatic Pneumothorax
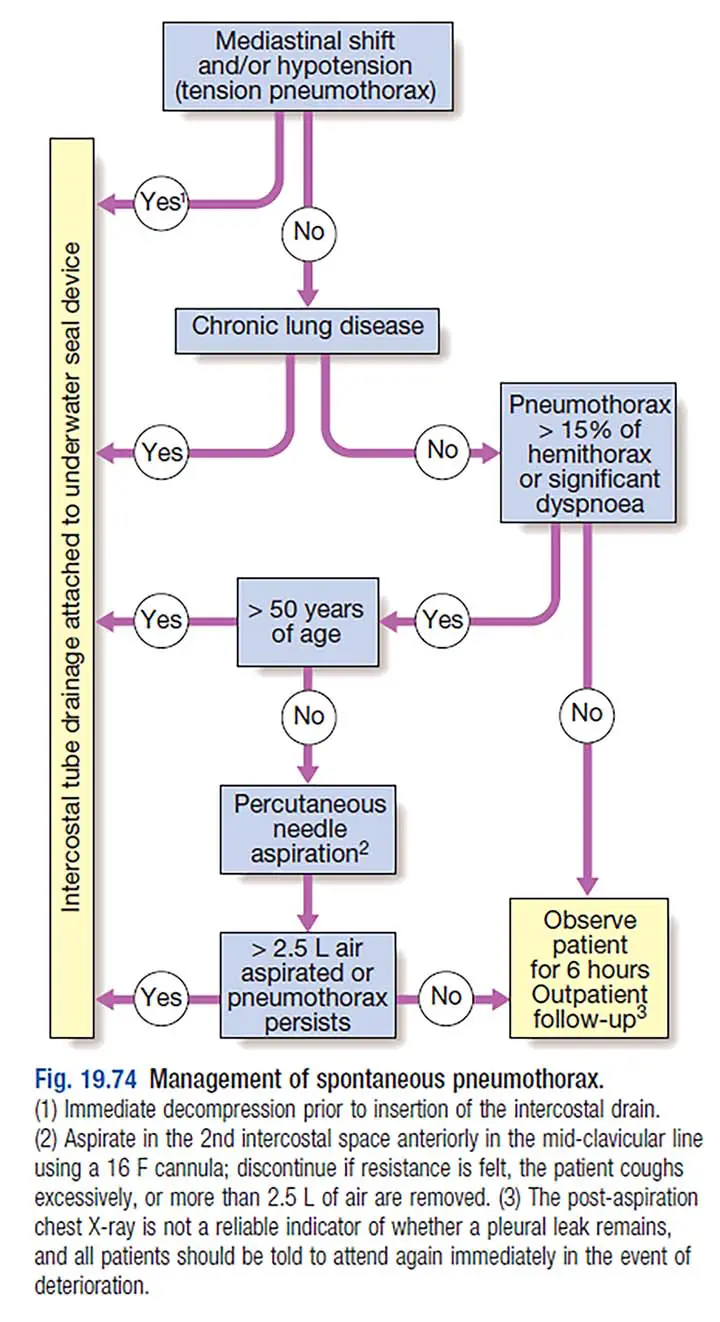
The scale of the pneumothorax, related co-morbid condition, whether it is open or closed, and whether it is plain or tension pneumothorax all influence management.
Methods for determining the proper size of a pneumothorax are debatable. If the lateral edge of the lung is more than 2cm from the thoracic cage, there are currently two methods listed in adults. This means that the pneumothorax is at least 50% and therefore high in scale. Calculate the ratio of the pneumothorax’s transverse radius (cubed) to the hemithorax’s transverse radius (cubed). Multiply the fraction size by 100 to get the percentage size.
The first step of treatment of pneumothorax(including traumatic)
All patients with chest injuries should have their airway, breathing, and circulation tested. Since pericardial tamponade can cause signs and symptoms identical to tension pneumothorax, the patency of the airway and the adequacy of the ventilatory efforts should be assessed along with the integrity of the chest and the circulatory status. If there are no contraindications, such as a spinal fracture, upright positioning can be helpful.
Sucking chest wounds(penetrating wounds) need immediate coverage with an occlusive or pressure bandage made airtight with clean plastic sheeting. In an emergency, the sterile inside of a plastic bandage packaging may be used. Tension pneumothorax or other life-threatening respiratory emergencies can occur if a patient with a penetrating chest wound is left unattended.
In the case of a suspected tension pneumothorax, a thin needle may be used to alleviate the pressure and enable the lung to re-inflate. A pneumothorax that hasn’t been handled is an ultimate “no” for evacuation or air travel.
Hemothorax may occur in combination with pneumothorax, and the patient can need immediate intravenous infusion, necessitating the use of a large-bore iv cannula.
Providing Oxygen Therapy
100 percent oxygen should be administered right away. In both clinical and laboratory settings, supplemental oxygen increases the rate of pleural air absorption. When you breathe 100% oxygen instead of air, the alveolar pressure of nitrogen decreases, nitrogen is washed out of tissue, and oxygen is taken up by the vascular system. This creates a significant gradient between tissue capillaries and the pneumothorax space, resulting in a multifold increase in pleural space absorption. It is recommended that any hospitalized patient with a pneumothorax who is not undergoing aspiration or tube thoracostomy be given high-concentration supplemental oxygen. Normally, 1.25 percent of the volume is consumed every 24 hours, so 10% of the volume is absorbed after 8 days, 20% after 16 days, and so on.
The majority of patients with small pneumothoraces are treated with oxygen, and no further care is usually needed other than repeat chest X-rays(PA radiograph).
The use of needle aspiration and/or small-bore catheter positioning for the treatment of pneumothoraces has been endorsed in many prospective studies dating back to the mid-1980s in both emergency medicine and surgery publications.
Tube thoracostomy risks include death, lung or mediastinum damage, internal bleeding (usually from an intercostal artery injury), infection, bronchopleural fistula, and the insertion of a subcutaneous or intraperitoneal tube.
Simple Cannula Aspiration
Instead of the standard needle, which was connected with the possibility of lung laceration, it is done with a plastic iv cannula. The position of the second intercostal space in the midclavicular line is normal. To avoid life-threatening hemorrhage, it can also be done in the fifth intercostal space in the anterior axillary line. In selected patients, needle aspiration and/or small catheter insertion are efficient, convenient, secure, and cost-effective alternatives to thoracotomy, according to publications from the American College of Chest Physicians (ACCP) and the British Thoracic Society (BTS).
Tube Thoracostomy
If simple aspiration fails and thoracoscopy is not easily obtainable, this technique is recommended. The insertion site is the same as for simple aspiration. It induces rapid re-expansion of the underlying lung and does not necessitate a lengthy stay in the hospital. Since the risk of pulmonary edema from rapid re-expansion is higher, it is possibly best to use a water seal and avoid suction for the first 24 hours after tube thoracostomy. Malecot catheters are being phased out in favor of pre-packaged disposable plastic tubes with a long central metal trocar (18-24 Fr Gauge). The flow of bubbles during expiration and coughing, as well as the increase in the amount of fluid in the underwater seal during inspiration, indicate proper tube positioning.
If the lung has not expanded or if there is a recurrent air leak 72 hours after tube thoracostomy, thoracoscopy or thoracotomy should be considered.
Prevention of Traumatic Pneumothorax
- Stay focused and safe during physical sports such as football, rugby
- Advise people to use seat belts and other passive restraints when driving.
- If necessary, use the supraclavicular approach rather than the infraclavicular approach while cannulating the subclavian vein to reduce the chance of pneumothorax formation.
- Ultrasound instruction is preferred for transbronchial, transthoracic, and other procedures.
Few last words
Since ancient times, the state of Traumatic Pneumothorax has been known. Various diagnostic and treatment approaches are recommended from time to time. Traditional approaches to the diagnosis and management of pneumothorax are being questioned, and doctors should have an open mind when evaluating new treatments. CT scans’ function in diagnosing pneumothorax is improving and becoming more clearly established as they become cheaper and more commonly used. While there are more instances of small pneumothorax being diagnosed, management decisions are not generally changing. Many etiologies have less expensive and painful solutions (other than traditional tube thoracostomy and admission), and more patients are being discharged home than in the past. To have the best treatment for patients with pneumothorax, it’s crucial to understand these patterns.
Last Updated on February 23, 2022 by Learn From Doctor Team