Table of Contents
Tension Pneumothorax Overview
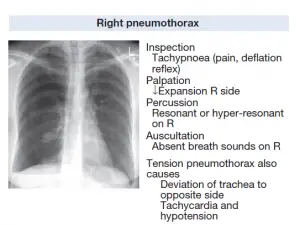
Tension Pneumothorax is a critical condition that can put your life at risk. Tension Pneumothorax occurs when the air becomes caught in the pleural cavity as a result of the chest wall or lung trauma or injury, it may cause a cascading effect that includes a rapid worsening of a patient’s ability to sustain oxygenation.
Tension Pneumothorax is a subtopic, to understand tension pneumothorax we’ve to study both Pneumothorax and Tension Pneumothorax at the same time.
Pneumothorax
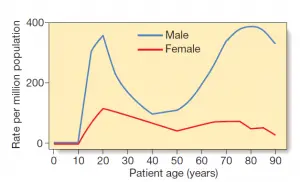
Pneumothorax is described as the presence of gas(air) in the pleural space, which may occur naturally or as a result of iatrogenic injury or trauma to the lung or chest wall. Patients who have no previous history of lung disease or abnormality may develop a primary spontaneous pneumothorax. Smoking, being tall, and having apical subpleural blebs are the most important risk factors. Patients with a previous history of lung disease are more likely to develop a secondary pneumothorax, which is linked to a higher mortality rate.
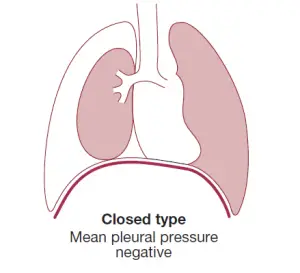
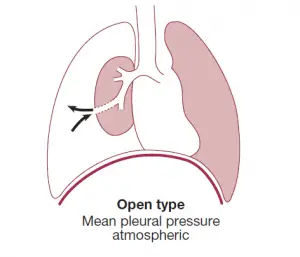
The pneumothorax is pointed as a ‘closed’ pneumothorax when the contact between the airway and the pleural space closes off when the lung deflates and does not re-open.
An ‘open’ pneumothorax, on the other hand, occurs when the contact fails to seal and air passes freely between the bronchial tree and the pleural area. A bronchopleural fistula is an example of the latter, which, if large enough, may promote infection transmission from the airways into the pleural space, leading to empyema. An open pneumothorax occurs when an emphysematous bulla, tuberculous cavity, or lung abscess ruptures into the pleural room.
What Is Tension Pneumothorax
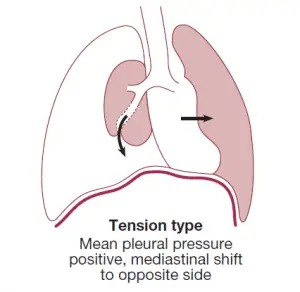
But sometimes, the airway-pleural space contact serves as a one-way valve, allowing air into the pleural space during inspiration but not out during expiration. Huge quantities of trapped air build up in the pleural space over time, causing the intrapleural pressure to rise well above atmospheric levels. A tension pneumothorax is what this is. The strain forces the mediastinum to the other side, compressing the opposite normal lung and impairing systemic venous return, placing the patient’s life at risk.
Don’t ever think a tension Pneumothorax is causing from the patient’s psychological tension or stress.
Classification of Pneumothorax
Spontaneous Pneumothorax
Primary Pneumothorax
- There is no previous history of lung disease. The pulmonary part of a pleural adhesion or the breach of a small pleural bleb allows gases to pass from the lung into the pleural area.
Secondary Pneumothorax
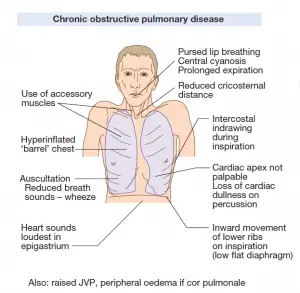
- COPD (Chronic Obstructive Pulmonary Disease) and tuberculosis are the most common underlying lung diseases; asthma, lung abscess, pulmonary infarcts, bronchogenic carcinoma, and all types of fibrotic and cystic lung disease are also common.
Traumatic Pneumothorax
- Iatrogenic: (History of Thoracic Surgery or Biopsy)
- Chest wall injury
Causes of Tension Pneumothorax and Traumatic Pneumothorax
- Subclavian or Internal jugular vein catheterization
- Biopsy of the lung
- Barotrauma(develop due to positive pressure ventilation)
- Thoracentesis
- Pacemaker insertion
- Bronchoscopy
- Tracheostomy(Percutaneous)
- Intercostal nerve block
- Cardiopulmonary Resuscitation
- Trauma (Penetrating or blunt force)
- Rib Fracture
Tension Pneumothorax can be associated with other causes;
- Spontaneous Pneumothorax(Idiopathic)
- Open Pneumothorax
- Spontaneous Pneumothorax converted into Tension Pneumothorax
Epidemiology of Tension Pneumothorax
Pneumothoraces(Pleural of pneumothorax) caused by trauma or tension are more common than spontaneous pneumothoraces. Iatrogenic pneumothorax is most commonly caused by transthoracic needle aspiration and catheterization. Iatrogenic pneumothoraces are becoming more common in US hospitals as intensive care modalities such as positive pressure ventilation and catheterization become more common. When inserted in the internal jugular or subclavian, central venous catheterization raises the risk of pneumothoraces. The incidence ranges from 1 to 13%, but if several attempts are made, the rate rises to 40%. If operations are performed using ultrasound, the numbers are lower. Iatrogenic pneumothorax typically results in significant morbidity, although death is uncommon. It’s about 0.05%.
Tension pneumothoraces can develop in 1 to 2% of cases that start out as idiopathic spontaneous pneumothoraces. It’s difficult to know how widespread tension pneumothorax is because by the time trauma patients arrive at trauma centers, they’ve already had decompressive needle thoracotomies. An associated pneumothorax or tension pneumothorax occurs 20% of the time in trauma patients. A pneumothorax is associated with serious chest trauma 50% of the time. The likelihood of a traumatic pneumothorax is proportional to the size and mechanism of the injury. According to a report of military deaths caused by thoracic trauma, up to 5% of combat casualties with thoracic trauma had stress pneumothorax at the moment of death.
Clinical Features of Pneumothorax
Sudden onset unilateral pleuritic chest pain or shortness of breath are the most common symptoms. Shortness of breath may be serious in people who have underlying chest disease, and it does not go away on its own. A physical examination can be common in patients with a minor pneumothorax. Breath sounds are reduced or absent when the pneumothorax is high (> 15% of the hemithorax). Pneumothorax is diagnosed by the absence of breath sounds and a resonant percussion tone.
Clinical Features of Tension Pneumothorax
In a tension pneumothorax, on the other hand, shortness of breath develops quickly and is accompanied by tachycardia, hypotension, cyanosis, and tracheal relocation apart from the silent hemithorax.
If the mediastinum has been splinted by malignant disease or scarring, tension pneumothorax may develop without mediastinal change.
Investigations For Pneumothorax
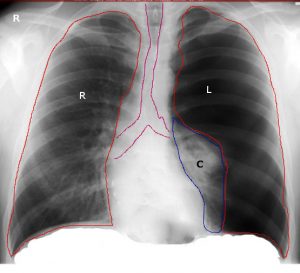
The deflated lung’s sharply outlined edge is visible on the chest X-ray, with full translucency (no lung markings) between itself and the chest wall. It’s important to distinguish between a pneumothorax and a broad preexisting emphysematous bulla. In difficult situations, CT is used to prevent misdirected aspiration attempts. X-rays will also show any pleural fluid or underlying pulmonary condition, as well as the degree of any mediastinal shifting.
Differential Diagnosis of Pneumothorax
- Pulmonary Embolism
- Acute aortic dissection
- Pneumonia
- MI(Myocardial Infarction)
- Acute Coronary syndrome
- Acute Pericarditis
- Rib Fracture
- Injury of the Diaphragm
- Oesophageal Spasm
- Costochondritis
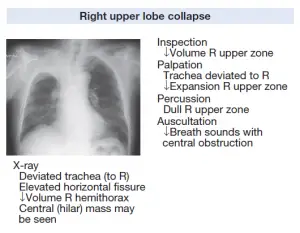
Tension Pneumothorax X-ray

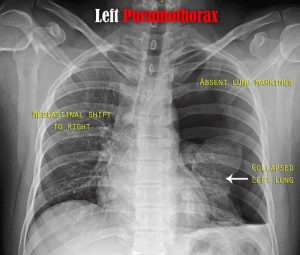
Read Pneumothorax X-ray: Radiological Diagnosis of Pneumothorax
Treatment and Management of Tension Pneumothorax
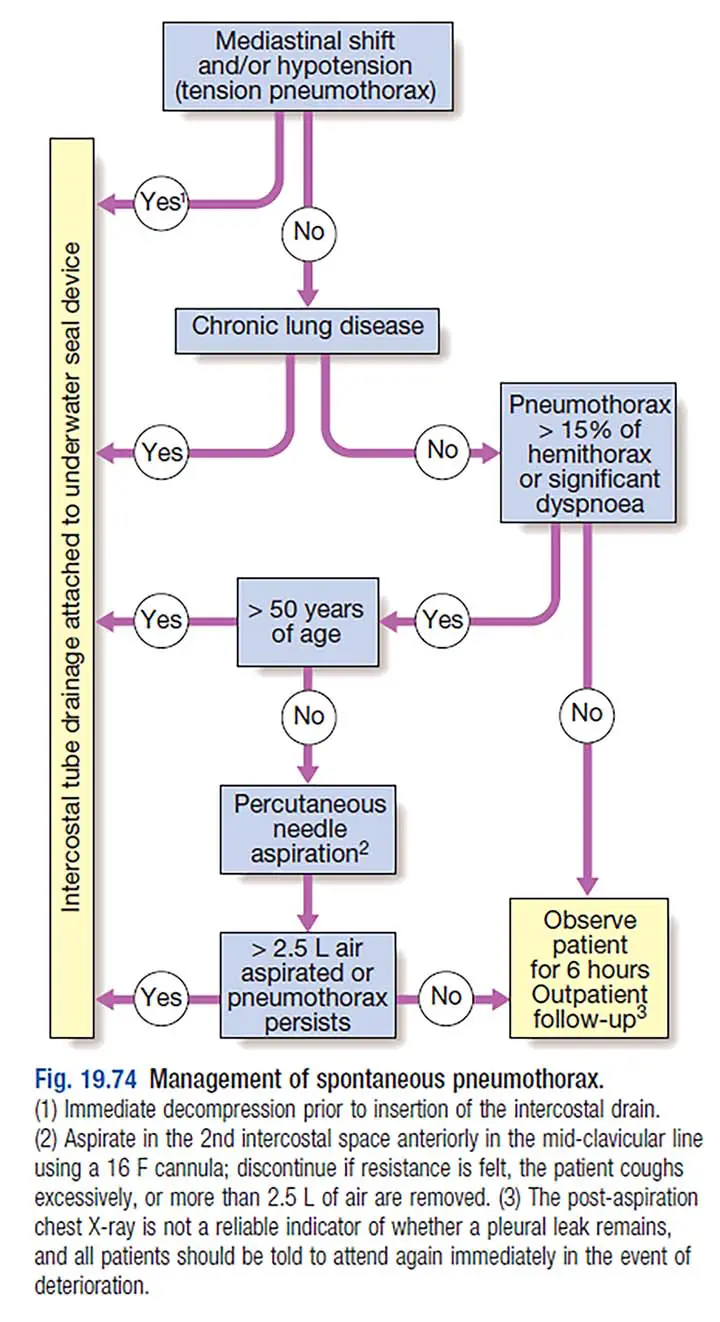
When the lung edges are less than 2 cm from the chest wall and the person is not short of breath, a primary pneumothorax typically resolves without treatment. Percutaneous needle aspiration of gas(air) is a quick and well-tolerated alternative to intercostal tube draining in young patients with a moderate or broad spontaneous primary pneumothorax, with a 60–80% chance to avoid the need for a chest drain.
Secondary pneumothorax, on the other hand, may cause respiratory distress in patients with severe underlying chronic lung diseases or conditions. Aspiration efficiency is much less in these patients, and intercostal tube drainage and inpatient monitoring are typically needed, particularly among those over 50 years old and those with respiratory compromise. If a tension pneumothorax occurs, removing the positive pressure as soon as possible with the insertion of a blunt cannula into the pleural space can be helpful, allowing time to plan for the insertion of a chest drain.
Intercostal drains are mounted in the 4th, 5th, or 6th intercostal spaces in the mid-axillary line, attached to an underwater seal or one-way Heimlich valve, and safely secured to the chest wall when necessary. Clamping an intercostal drain is a highly hazardous technique that is only used in extreme situations. After the lung has completely re-inflated and the bubbling has ceased, the drain should be removed the next morning. If the bubbling persists after 5–7 days, surgery is recommended. If the drainage bottle’s bubbling ceases until it re-inflates completely, the tube is either blocked, kinked, or displaced. Supplemental oxygen has been shown to accelerate resolution by speeding up the rate at which nitrogen is absorbed by the body(pleura).
Patients with a closed pneumothorax do not travel by airplane because the trapped gas expands as they increase in altitude.
There is no clear evidence to show how long patients can postpone flying after the complete resolution, but guidelines recommend waiting 1–2 weeks with the assurance of maximum inflation before flying. Patients should be persuaded to quit smoking and notified about the hazards of a persistent pneumothorax.
Unless surgical pleurodesis has secured the lung to the chest wall, diving can be risky after a pneumothorax.
Recurrent Spontaneous Pneumothorax
Recurrence of primary spontaneous pneumothorax affects approximately 25% of patients within the first year of either aspiration or tube drainage, which may prompt definitive care. Following a second pneumothorax, surgical pleurodesis is prescribed in all patients, and it should be considered after the first episode of secondary pneumothorax if low respiratory reserve renders recurrence dangerous. Pleurodesis can be accomplished by thoracotomy or thoracoscopy with pleural abrasion or parietal pleurectomy.
Facts about Needle Decompression(Aspiration) to manage Tension Pneumothorax
To perform a needle decompression successfully, you must have the correct equipment on hand. According to the latest study, a 3.25 inch 14 gauge (or greater diameter) needle is the safest needle for treating a tension pneumothorax in adult patients. However, existing teachings may be unsuccessful in treating a tension pneumothorax successfully. For chest decompression, a 1.75 to 2 inch, 14 to 16 gauge needle is used. Recent studies have shown that this needle length is inadequate for patients with a tension pneumothorax.
CT scans were used to assess the thickness of the chest wall in a study conducted in Prehospital Emergency Care. Based on the body structure studied, it was determined that using a 1.75-inch needle catheter for chest decompression would result in a 50% failure rate.
Recent research published in the Journal of Trauma discovered that using a 2-inch catheter, as is widely taught, resulted in a failure rate of just over 35% of the population.
In a research published in Military Medicine, a needle with a length of 3.25 inches successfully entered the pleural space in 99 percent of the people tested. Keep in mind that needle length is crucial for removing trapped air, and patients are often larger than they were previously.
The specific management of tension pneumothorax has also been the subject of research at the US Army Institute of Surgical Research. According to research, chest decompression with a 14 gauge needle is just as effective as a chest tube in treating a strain pneumothorax, and the therapeutic effects will last 3 – 4 hours.
If you’re using a needle catheter with a flash chamber, make sure it’s taken out. There are needles specifically designed to treat a tension pneumothorax. There are no flash chambers on these prepackaged 3.25-inch 14 gauge needles. The replacement of the chamber means that the provider does not have to remember to remove it in a high-stress situation. It has been stated that the provider sometimes forgets to remove the flash chamber, resulting in the procedure failing.
Performing Needle Decompression(Aspiration) to manage Tension Pneumothorax
If the patient has a tension pneumothorax, a needle decompression should always be done. The needle should be inserted at a 90-degree angle to the chest wall when applied. This is an essential move because it will put the needle straight into the pleural space. If some other angle is used, other structures in the region, such as major blood vessels or even the heart, may be damaged.
The measures for performing a chest decompression are as follows. You should, however, stick to your procedures.
- If at all necessary, make sure the patient is getting enough oxygen.
- Choose the right spot: the second intercostal space and the mid-clavicular line on the affected side. Note: From the nipple to the clavicle, draw an imaginary line. The needle should not be closer than this line to the center of the chest.
- Clean the region with rubbing alcohol or a povidone solution.
- Prepare the needle; it will need to be removed if it has a leur-lock or flash chamber.
- Insert the needle into the second intercostal space, just over the third rib, at a 90-degree angle to the chest. Blood vessels can be seen flowing around the bottom of the ribs. In the intercostal space, make sure the needle is closer to the top margin of the lower rib. This will ensure that these vessels are not hurt.
- Listen for a blast of air leaving the needle.
- Remove the needle and keep the catheter in place, ensuring that the needle is properly disposed of.
- Use tape to keep the catheter in place. Some people recommend covering the catheter’s end, but this will depend on the particular.
- Ascertain that the patient’s health has changed and that the anxiety has been eased. If the condition does not change, the operation must be performed with a second needle inserted next to the first.
- The patient should be tracked and then reassessed.

Prognosis of Tension Pneumothorax
To prevent more morbidity and death, tension and traumatic pneumothoraces must be treated right away. A poor prognosis is related to a delay in treatment and management. Tension pneumothorax can be caused by a number of factors and, if left untreated, can lead to respiratory insufficiency, cardiovascular failure, and death. Recurrence in uncomplicated pneumothoraces can happen anywhere from six months to three years. Smokers, COPD patients, and AIDS patients are more likely to experience recurrences.
Possible Complications of Tension Pneumothorax
- Respiratory Failure
- Cardiac Arrest
- Pneumopericardium
- Pneumoperitoneum
- Bronchopulmonary Fistula
- Hemothorax
- Neurovascular bundle damage due to Thoracotomy
- Skin infection in the site of Thoracotomy
- Empyema
- Pyopneumothorax
Whom should you consult(For Patients)
- Thoracic surgeon
- Pulmonologist
- Interventional radiologist
- Intensivist
Few Last Words About Tension Pneumothorax
A tension pneumothorax is a potentially fatal condition. It can manifest as a closed or open chest injury. If the patient has an open chest wall trauma, the care practitioner must be mindful that a tension pneumothorax is a distinct possibility. It’s important to have good assessment skills, the right tools, and the experience to efficiently alleviate a stress pneumothorax to save patients’ lives.
Last Updated on February 23, 2022 by Learn From Doctor Team