Table of Contents
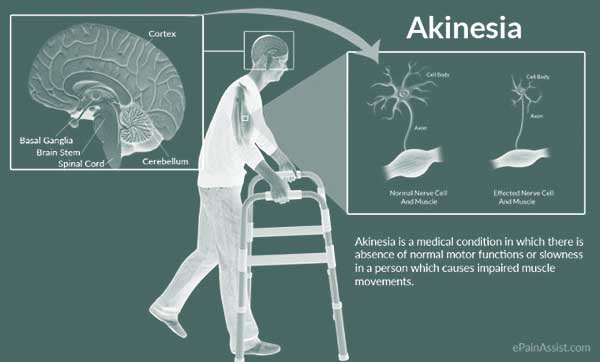
What is Akinesia?
The word akinesia refers to the inability to move your muscles willingly. It’s most often thought to be a characteristic of Parkinson’s disease (PD). It may also manifest as a symptom of other illnesses.
“Freezing” is one of the most common symptoms of akinesia. As a consequence of a neurological disorder like Parkinson’s disease, one or more parts of the body couldn’t longer move. Motor neurons (nerve cells) in your brain’s movement centers weaken and die as a result of these conditions. The neurons would then be unable to transmit signals to the nerves and muscles. You can lose control of your muscles as a result of this. This includes muscles in your face, hands, legs, and other muscles that you use on a daily basis.
Akinesia, like many of the disorders that cause it, is a chronic disease. The bulk, but not all, of the diseases, are progressive and incurable. The akinetic syndrome is a reversible condition caused by severe hypothyroidism. Parkinsonism caused by drugs can also be reversible.
There are treatments and drugs available to help delay the development of akinesia and neurological disorders like Parkinson’s disease. They might be able to lessen the impact of akinesia on your everyday life.
What is Fetal Akinesia?
A fetus in the womb may develop akinesia. Fetal akinesia is the medical term for this disease. Fetuses in these situations do not shift as much as they should. Other symptoms may accompany this condition. The lungs of a fetus may not grow properly, or the baby may have irregular facial features when born. The fetal akinesia deformation series is the name for these signs (FADS). It’s most likely due to their genetics.
Symptoms of Akinesia
The following are some of the signs of akinesia:
- When a person first begins to walk anywhere, it can be difficult.
- The rigidity of muscles, normally starting with the neck and legs. Face muscles may become rigid, resembling a mask.
- Unable to move the feet properly, particularly when turning or approaching a destination, all of a sudden.
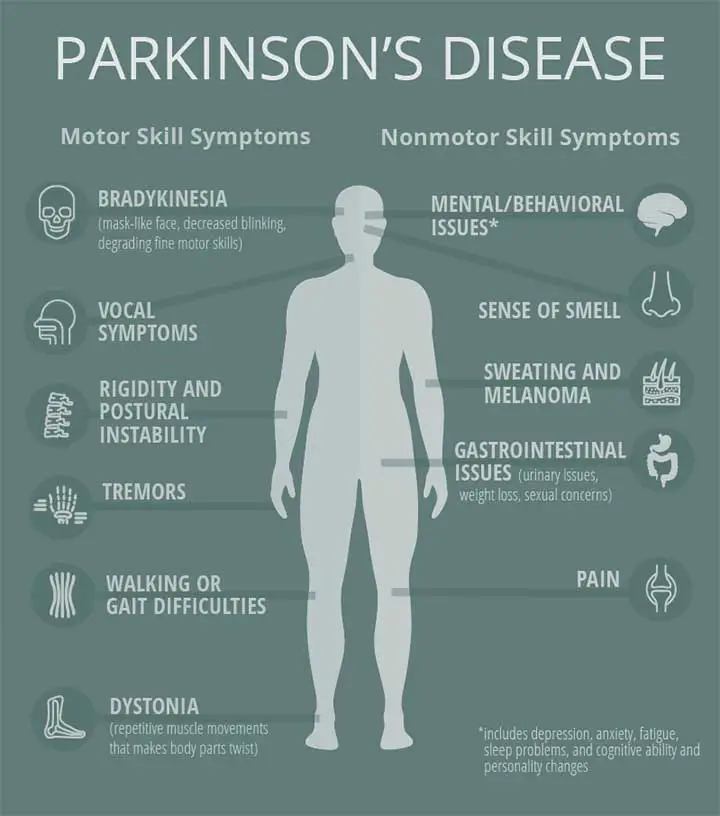
The signs of Parkinson’s disease are not the same for everyone. The word TRAP is often used by doctors to identify the symptoms of Parkinson’s disease. These letters stand for:
- Tremor at rest
- Rigidity
- Akinesia
- Postural instability
It’s also conceivable that a person can develop akinesia without having any other symptoms of Parkinson’s disease.
“Pure” akinesia with so-called gait-freezing is one such case of akinesia. This symptom is not accompanied by resting tremors, generalized slower movements, or rigidity, which are all common Parkinson’s symptoms.
Akinesia Vs Dyskinesia
Dyskinesia is not the same as akinesia. Dyskinesia is a disorder in which the muscles twitch or shift without your permission. You can’t steer your muscles to move if you have akinesia (sometimes entirely). The muscles, on the other hand, do not lose their skills. The extrapyramidal structure, also known as movement centers, is malfunctioning.
Your muscles can move randomly or continuously in dyskinesia, and you may not be able to stop them. Dyskinesia, like akinesia, can occur in Parkinson’s disease.
Causes of Akinesia
Parkinson’s disease – This causes the brain to generate less dopamine, impacting a person’s ability to regulate their muscles.
Medication-induced – Parkinson’s-like symptoms occur when a person takes too much dopamine-inhibiting medication.
Progressive supranuclear palsy (PSP) – is a progressing brain disease that typically affects coordination during walking.
Thyroid hormone levels – Hypothyroidism or extremely low thyroid hormone levels may cause akinesia.
Men with Parkinson’s disease seem to be more likely than women to have akinesia. People who seem to have a resting tremor as their primary symptom of Parkinson’s disease are less prone to developing akinesia than those who do not.
Treatment Procedure
Certain Medications
A combination of levodopa, a central nervous system agent, and carbidopa is one of the most effective therapies for akinesia caused by Parkinson’s disease. Carbidopa reduces the severity of levodopa’s side effects, such as nausea.
Lack of dopamine can cause akinesia in people with Parkinson’s disease. Dopamine is produced in your brain and then transported throughout your body through neurons. Since the brain converts levodopa into dopamine, it helps to treat akinesia and other PD symptoms. It can then be taken into the body to help alleviate muscle weakness associated with akinesia, as well as tics and tremors associated with other PD symptoms.
Carbidopa and levodopa can interact with other drugs and have serious side effects. Before you start taking these drugs, talk to your doctor about how this procedure can affect you.
MAO-B inhibitors also prevent dopamine from being degraded by the body’s enzymes naturally. This also boosts the amount of dopamine available to fight akinesia and delay the progression of Parkinson’s disease.
In most cases, medications are ineffective in treating akinesia caused by PSP. Antidepressants can help with the akinesia and depression that can accompany PSP. Botulinum toxin injections can also help with symptoms including involuntary eyelid closure (blepharospasm).
OTC Drugs
Pressure and stiffness can be caused by akinesia, and taking PD or PSP drugs can also cause pain and discomfort. Taking over-the-counter pain medications like ibuprofen and acetaminophen, which are nonsteroidal anti-inflammatory drugs (NSAIDs), can help alleviate some of the pain that PD, PSP, and their related medications can cause.
Stimulators
Doctors may explore the possibility of surgically implanting electrodes to stimulate movement centers if traditional medications wear off too quickly or do not have the desired effect on akinesia. In more extreme cases, this therapy may assist with symptoms. Deep brain stimulation is the term for this. It’s a PD technique that’s becoming increasingly popular.
Home Remedy
Regular exercise can help you cope with the pain and discomfort that can accompany akinesia and other motor function issues caused by PD or PSP. Depending on your symptoms and the development of akinesia, talk to your doctor or a physical therapist about developing an exercise schedule that is relaxed and healthy for you. It is important that you do not overexert yourself or fall while exercising. Stretching the muscles with yoga or tai chi will help delay the development of akinesia. Exercise has been shown to help people with Parkinson’s disease postpone the onset of functional decline.
If you’re in the early stages of PD or PSP, taking coenzyme Q10 for several months can help. Drinking plenty of water (at least 64 ounces a day) and eating high-fiber foods will help keep the symptoms to a minimum.
Massages and acupuncture are two treatments that can help you relax your muscles and alleviate the symptoms of PD and PSP. Meditating or relaxing things like listening to music or painting will help you slow down the symptoms of akinesia and keep control of your muscles.
Prognosis
Although there is no cure for adult-onset akinesia, symptomatic treatment can significantly improve these patients’ quality of life. Although mild akinesia does not directly result in death, severe akinetic crises can cause dysphagia, autonomic dysfunction, and aspiration, all of which can be fatal.

Fetal akinesia syndrome has been found to be primarily lethal in utero, with 30% of fetuses stillborn. The final prognosis is determined by the underlying cause. The majority of live-born infants die within the first month of their lives. This could justify an offer for late-term abortion in countries where it is legal.
Risk Factors
- A history of bradykinesia (slow muscle movements)
- Having Parkinson’s disease for a long period of time
- Instability of posture
- Muscle rigidity problems
Doctors have also identified two gene mutations linked to an increased risk of fetal akinesia.
If a person has a history of the condition in family members or babies, they should consult a genetic specialist. This allows them to be tested for the gene mutations DOK7 and RAPSN, which are linked to akinesia.
This section is for Doctors and healthcare professionals. Others may find this section difficult to understand.
Epidemiology
Akinesia in clinically observed parkinsonism has been linked to the motor variant of frontotemporal lobe dementia (FTLD) rather than PD-related frontal degeneration. Around 30% of patient populations with clinically confirmed FTLD had parkinsonian symptoms, most notably rigidity or akinesia. Acute akinesia is a relatively uncommon occurrence that occurs in 0.3 percent of Parkinson’s disease patients as a result of infectious pathology or other stressors.
Akinesia is frequently associated with fetal akinetic syndrome in the pediatric age group. This is linked to a high rate of intrauterine mortality. The incidence in live births, on the other hand, is one in every 3,000 cases, with over 320 genes implicated in its pathology. It predominates in Asian, European, and African communities.
Pathophysiology of Akinesia
The pathogenesis of akinesia in adults appears to be primarily caused by pallidonigroluysian degeneration, which primarily results in freezing. The specific pathology, however, is determined by the type of akinesia. It is most likely related to PSP in cases of pure akinesia with gait freezing without any other symptom or diagnosis of PD. PSP is associated with evidence of degeneration in the subthalamic nuclei, globus pallidus, and substantia nigra.
The primary cause of akinesia in Parkinson’s disease patients appears to be a dysfunction in phasic and tonic dopamine release. In contrast, resting tremors are caused primarily by a dysfunctional tonic phase of dopamine release. Another theory proposes that akinesia in Parkinson’s disease patients is caused by bilateral frontal involvement and is accompanied by worsening mental states.
Fetal akinesia has been linked to approximately 320 genetic variations, all of which could manifest as this syndrome. The pathology is visible at all levels, including the brain, spinal cord, motor neuron, neuromuscular junction, and muscle.
Diagnosis
A patient’s akinesia is diagnosed clinically and is marked by a delay or inability to respond or perform a motor command. Reaction time tests are used to quantify the degree of akinesia. It usually shows a delay in simple reaction time but a normal choice reaction time.
The following neuroimaging studies are used to evaluate akinesia:
- MRI stands for magnetic resonance imaging (MRI)
- MRI for functional purposes
- Single-photon emission computed tomography is a type of computed tomography that uses a single photon
- Positron emission tomography is a type of positron emission tomography.
In patients with akinesia-rigidity prominent Parkinson’s disease, the left inferior frontal gyrus, right middle frontal gyrus, and right superior frontal gyrus have a higher global functional connective density (FCD) than the tremor-dominant variant, while the left cerebellum anterior lobule has a lower global FCD.
Imaging outcomes in pure akinesia with gait freezing, which is associated with PSP, show strong cortical thinning in the inferior bilateral frontal, left orbitofrontal, right anterior cingulate, bilateral insula, bilateral supramarginal, right angular and precunial, and bilateral temporal areas, frequently involving the parahippocampal and lingual gyri. The old and medically used hummingbird sign or the morning glory sign, with loss of the lateral convex margin of the tegmentum, can be seen on MRI. On histopathology, patients have diffuse Tau protein aggregates in the basal ganglia.
The modern imaging techniques provide no data on the neurotransmitter type involved in the pathogenesis of the disorder. Futuristic models are likely to use pharmacological imaging, complex behavioral tasks, and movement analytical tools to quantify the akinesia.
After acquiring a normal karyotype and ruling out other conditions, a presumptive diagnosis of fetal akinesia is formed. After clinically presenting with reduced fetal movement, fetal edema, or fixed limb posturing as seen on antenatal ultrasonography, an antenatal diagnosis can be made as early as 12 weeks of gestation.
Management
Adult akinesia treatment focuses on slowing the progression of the disease process. Akinesia is treated symptomatically rather than curatively.
- Drug therapy: In Parkinson’s disease patients, this primarily aims to modify/supplement the impaired dopamine release.
- Progressive resistance exercise can help patients with an akinetic rigid variant of Parkinson’s disease improve their symptoms of improved static posturography, gait, and overall quality of life.
- Deep brain stimulation is the most researched surgical procedure for the treatment of akinesia. It is typically used to improve dopamine secretion and symptoms of tremors, akinesia, and rigidity.
- Thalamotomy, pallidotomy, neural implants, and electrical stimulation are other procedures used in severe cases.
The treatment for fetal akinesia is primarily supportive, owing to the poor prognosis in a live birth. Initially, resuscitation measures are used to combat pulmonary hypoplasia. Initially, medications such as sildenafil and iloprost are used to control elevated pulmonary pressures. After adequate discussions with the parents, they can still be converted to a less life-sustaining comfort care approach. Antimicrobials may be necessary. Due to gut malrotation, short-gut syndrome, and impaired swallowing, these patients frequently require prolonged parental nutrition. Anticonvulsants and thyroid hormone replacement are used to treat central nervous system abnormalities such as seizures and endocrine disorders such as hypothyroidism.
Differential Diagnosis
- Catatonia
- Akinesia arrest reaction
Differential Diagnosis of Fetal Akinesia
- Osteogenesis imperfecta
- Potter’s sequence
- Congenital myasthenia gravis
- Antibodies to the fetal acetylcholine receptor in mothers
- Metabolic disorders
- Trisomy 18
Complications
Pulmonary
- Pulmonary hypoplasia,
- Pulmonary hypertension
- Aspiration pneumonia
Neurological
- Seizures (Read Seizure Precautions for more information)
- Hypothalamic dysfunction.
Endocrine
- Hypothyroidism
- Hypothalamic dysfunction etc.

Akinesia Summary
The inability to perform a clinically perceptible movement is referred to as akinesia. It can manifest as a delayed response, a freezing in mid-action, or even complete immobility. Akinesia occurs when movement is not perceived because the amplitude of the movement is small or the time required to initiate the reaction is significantly increased. The former is frequently the result of severe bradykinesia, which is commonly misunderstood as akinesia. This makes distinguishing between the two difficult. Akinesia is characterized by a failure to rapidly accumulate sufficient power to initiate movement.
Last Updated on February 23, 2022 by Learn From Doctor Team